All published articles of this journal are available on ScienceDirect.
Can a ‘3-tier Screening’ Strategy be Adopted during COVID-19 Pandemic for Safer Air Travel and to Help Curb its Spread Across Borders?
Abstract
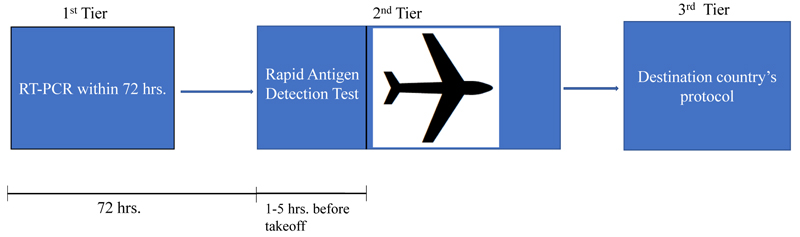
Since the appearance of SARS-CoV-2 in 2019, it spread quickly crossing geographical borders and thus affected almost the entire world. It was alarming to note its quick spread, which obviously was due to the increased frequency and ease of air travel in this era. Currently, many airlines (and countries too) have a prerequisite to have a negative COVID-19 RT-PCR test within 72 hrs. prior to boarding the flight. Although all the necessary precautions are strictly enforced during air travel, there is still a possibility that a person with a negative COVID-19 test (RT-PCR) around 72hrs prior to boarding the flight would have an infection and that the person would pass it on to fellow passengers on board and thus can further spread SARS-CoV-2 infection into the community if robust action is not initiated. There is also a subconscious apprehension among the passengers that co-passengers may have an infection on board. This is especially worrisome seeing the appearance of new variants recently. Here I present the logistics for a ‘3-tier screening’ protocol (1st test by RT-PCR within 72hrs of the flight schedule, 2nd test by rapid antigen detection method 1-5hrs prior to flight schedule, 3rd test post-arrival or to follow the destination country post-arrival protocol), which would at least provide an extra filter to separate the recently identified positive cases and thus prevent the spread of this threatening disease across the borders.
1. INTRODUCTION
More than a year and a half have passed since the emergence of SARS-CoV-2 infection in December 2019 in the Wuhan Province of China [1]. The infection spread quickly crossing the borders and hence the COVID-19 was declared as a pandemic by WHO on March 11, 2020 [1].
However, during this pandemic, a big relief was the quick development of novel diagnostic tests and the quicker availability of potent vaccines. Different diagnostic tests are available ranging from established tests such as Real-Time PCR (RT-PCR) and immunological tests detecting antigen or antibody, to some recent novel tests based on CRISPR-Cas or nanomaterials-based detection tests [2]. The majority of labs utilize RT-PCR as a confirmatory diagnostic test which is also utilized to assess the viral load. On the other hand, immunological tests complement virus detection. Enzyme-Linked Immunosorbent Assay (ELISA) is commonly used for detecting antibodies (IgM or IgG) or for detecting SARS-CoV-2 antigens. Similarly, chemiluminescence immunoassays and lateral flow immunochromatographic assays are also frequently used [2]. Of these, lateral flow immunochromatographic assays detecting viral antigens are now considered as a point-of-contact test as a rapid diagnostic test [2].
Advancement in technology has recently witnessed the development of some novel tests such as based on Clustered Regularly Interspaced Short Palindromic Repeats (CRISPR)-Cas 12/13 systems. One such test for detecting SARS-CoV-2 infection is STOPCovid, i.e., “SHERLOCK testing in one pot COVID”, which is based on lateral-flow/fluorescence-based assay and utilizes CRISP-Cas 13 system (where SHERLOCK= specific high-sensitivity enzymatic reporter unlocking) [2-4]. Interestingly, more recently, there are diagnostic approaches developed utilizing meta sensors [5].
Following the availability of a battery of diagnostic tests, including point-of-care rapid tests, different countries and airline operators have opted for their respective screening strategies to curb the spread of SARS-CoV-2 across borders. Air travel was considered as one of the important reasons for its wider geographical spread. Subsequently, borders were closed by many countries for a significant period when ultimately many of the countries had to reopen their borders due to obvious reasons. On the other hand, some countries have even not opened yet their borders fully for passengers from many countries, instead, they have created travel bubbles with few destinations.
While the flights resumed, all necessary precautions, including the use of face masks, appropriate distancing between passengers and hand sanitizing, etc. were strictly enforced. Moreover, a pre-requisite of negative COVID-19 test (by RT-PCR) within 1-3 days of boarding the flight was introduced by most of the airlines. Additionally, some countries are following a protocol of testing for COVID-19 on arrival (with an additional test after a few days). This somehow aligns with the Centers for Disease Control and Prevention (CDC) recommendations i.e., 1) to get tested 1-3 days prior to flight, 2) to get tested 3-5 days after travel and a homestay for 7 days after travel. CDC further suggested that if the post-test is a negative stay at home for full 7 days, and if the post-test was not performed, then stay for 10 days after the travel [6].
Realizing the fact that symptom-based screening is of limited value, The Government of the United States (GUS) has recently adjusted the entry strategy for international travelers [7]. Considering the fact that the transmission may occur from persons who either have no symptoms, or have not yet developed them, hence shifted the strategy more towards individual passengers focusing more on pre-departure, in-flight, and post-arrival health education, voluntary collection of contact information, minimizing crowding by enhancing electronic data collection and so on [7].
Some other countries, such as New Zealand, even had a more robust approach in safeguarding the citizens by implementing a protocol of having mandatory quarantine or isolation for 14 days in a managed facility for which the passenger has to obtain a paid coupon through pre-booking [8].
All these approaches are applaudable, however, there is still a possibility that a person who was negative for COVID-19 test around 72 hrs. prior to boarding the flight had an infection and this person might have recently started shedding off the virus on the day of boarding the flight. Said that, there is always a possibility that the person might transmit it to its fellow passengers on board, if not too many, at least a few of them. In most of the instances, if the passenger gets tested positive (here we call it as “dot-case”) after arriving at the destination, the co-passengers sitting closer to this Dot-Case (DC) are generally considered as contacts and then traced. Usually, we ignore that the DC might have roamed around inside the aircraft and thus might have exposed the passengers sitting even far from his/her seat. In this way, there are chances that the DC has also transmitted infection to these passengers sitting afar. If we had not tested every passenger in the aircraft post-arrival, there is always a remote possibility that some of the co-passengers could not be traced properly. Also, whatever passengers are tested as contact, they may not come out positive so early. There is always a possibility that the infection can be transmitted into the community by any of these passengers by the time robust measures are initiated. This situation could become grave seeing the emergence of new variants recently [9].
On top of all, there is always an apprehension in passengers, many times at subconscious level, that the fellow passengers sitting in the vicinity might have an infection. So, keeping this in mind, here I present the logistics for a ‘3-tier screening’ protocol by performing 3 separate tests at three different points of time; which includes the introduction of rapid testing (based on the principle of antigen detection) which is to be made mandatory for all the passengers just before boarding the flight. The rapid test is not expensive, does not require additional expertise, and moreover, the results are available in 10-20 mins. Normally, the passengers are called to airports 3 hrs. prior to the scheduled flight time. This pre-boarding testing can easily be handled by respective airlines before issuing the boarding passes. Considering the time constraints (if any), passengers may be asked to arrive airport 4-5 hrs. prior to departure so that all may be tested comfortably. This approach will provide an “extra filter” and thus a person who started shedding the virus recently, after his first negative test, may be prevented from spreading it further to fellow passengers and thus crossing the borders easily. Moreover, there would be lesser apprehension in passengers flying when they are aware that the test has been done recently and the fellow passengers are tested negative. There is always a possibility of false positivity and false negativity which is still debatable. A recent editorial in a reputed infectious disease journal also anticipates regular use of COVID-19 rapid test for crew members and passengers [10]. It is understood that there is nothing like full proof, but this approach of ‘3-tier screening’ by performing 3 separate tests at three different points of time perhaps would provide an extra filter in segregating the cases, which recently turned positive and thus help in curbing the spread of this threatening disease across the borders [7].
The application strategy for this ‘3-tier screening’ protocol and the time frames for the tests are summarized below and in Fig. (1):
1) 1st test by RT-PCR within 72 hrs. of the flight schedule.
2) 2nd test by rapid antigen detection method on the day of flight 1-5 hrs. prior to flight schedule.
3) 3rd test post-arrival (if the destination country has this protocol in affect) OR to follow the specific post-arrival protocol of the destination country.
CONCLUSION
COVID-19 pandemic knows no borders and air travel is one of the important reasons for its wider geographical spread. All the necessary precautions are strictly enforced by the airlines to combat this pandemic, but still, there is a possibility of spreading the infection to fellow passengers even though the passenger is negative for the COVID-19 (RT-PCR) test about 72 hours before boarding. As a result, the proposed “3-tier screening approach” in the current article could at least provide an additional filter to separate the recently identified positive cases, thus preventing the cross-border spread and contributing to flatten the COVID-19 pandemic curve. Moreover, introducing a screening step through a rapid test made mandatory, just prior to boarding the flight, will help alleviate fear and apprehension in travelers. Therefore, in an attempt towards limiting further spread of COVID-19, the introduction of this “3-tier screening” strategy globally could be a sincere effort towards curbing the spread of this deadly infection.
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
None to declare.
ACKNOWLEDGEMENTS
The secretarial support provided by Mr. Tomy Kaitharath, especially in preparing the figure, is highly appreciated.


