All published articles of this journal are available on ScienceDirect.
Management of Rhegmatogenous Retinal Detachment during COVID-19 Pandemic
Abstract
Patients with primary Rhuegmatougenous Retinal detachment during COVID-19 pandemic were more likely to present late, have macula involving disease secondary and to show poor visual outcomes. Pneumatic Retinopexy (PR) is a procedure that eliminates the need for admission and limits the duration of contact with patients. Hence, more feasible during periods of shortage in hospital beds and medical personnel in the pandemic. In our experience, we successfully performed pneumatic retinopexy on two confirmed COVID-19 cases with favourable visual outcomes. We would recommend retina surgeons be familiar with such procedure as it may be a good alternative to conventional treatment while minimizing the risk of transmitting COVID-19.
1. INTRODUCTION
The physical distancing restrictions during the Coronavirus Disease 2019 (COVID-19) pandemic had significant socioeconomic and health impacts [1]. In Saudi Arabia, the first COVID-19 case was reported in the eastern region in March 2020.
Ophthalmological services had the most significant reduction when compared to the other specialties [2]. Patients with primary Rhegmatogenous Retinal Detachment (RRD) on this pandemic were more likely to have macula-off disease secondary to delay in seeking treatment, thereby showing poor visual outcomes [3]. To limit close contact with patients, infection control measures were taken, such as the use of Personal Protective Equipment (PPE), encouraging the use of telemedicine for non-urgent cases, and environmental and administrative control. Surgical services were limited to urgent and emergency cases while keeping infection measures in consideration [4]. During this challenging period, exploring other quick, less used surgical options, it plays a significant role in minimizing the risk of infection and providing satisfactory outcomes. Pneumatic Retinopexy (PR) is a procedure that eliminates the need for admission and limits the duration of contact with patients [5]. In our experience, we successfully performed PR on two confirmed COVID-19 cases needing only two encounters, which lasted significantly shorter than encounters required in a typical Pars Plana Vitrectomy (PPV) or scleral buckle procedure. This report emphasizes the effectiveness of PR in managing RRD cases through the COVID-19 era while limiting the risk of exposure.
2. CASE REPORT
2.1. Case 1
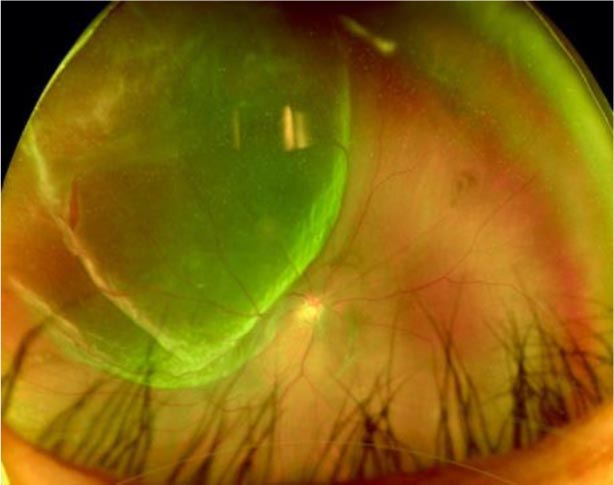
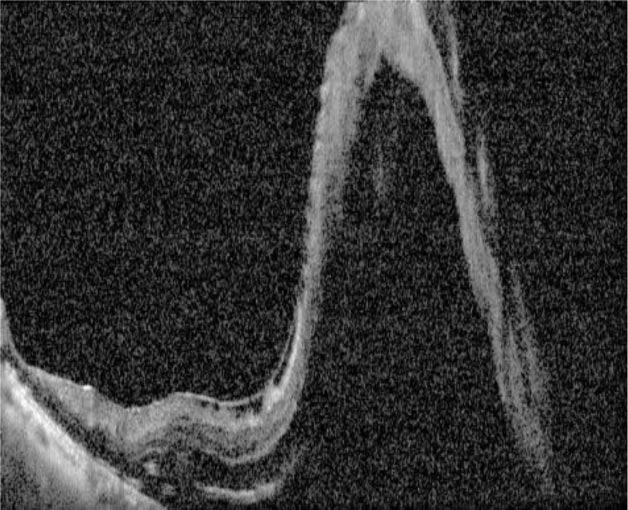
During the peak of the pandemic and major lockdown across Saudi Arabia. A 46 years old intensive care unit female nurse who was COVID-19 positive was referred to King Khalid Eye Specialist Hospital (KKESH) in Riyadh, Saudi Arabia, with the diagnosis of right eye acute Rhegmatogenous Retinal Detachment (RRD) for 1 day preceded by floaters and flashes in the right eye. She was a medically free myope with no history of trauma. Her Best-Corrected Visual Acuity (BCVA) and Intraocular Pressure (IOP) at presentation were HM OD; 20/25 OS, 13 mmHg OD; 14 mmHg OS respectively. Fundus examination revealed inferior organized vitreous hemorrhage with bullous superior-temporal RRD, macula off and Horseshoe Tear (HST) at 11 o’clock. A wide-field color fundus photograph was obtained, and Optical Coherence Tomography (OCT) confirmed macular detachment and showed attached posterior hyaloid (Figs. 1 and 2).
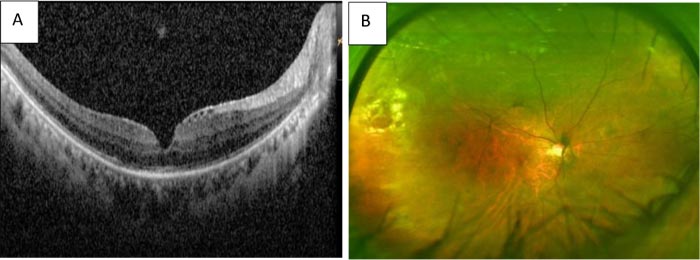
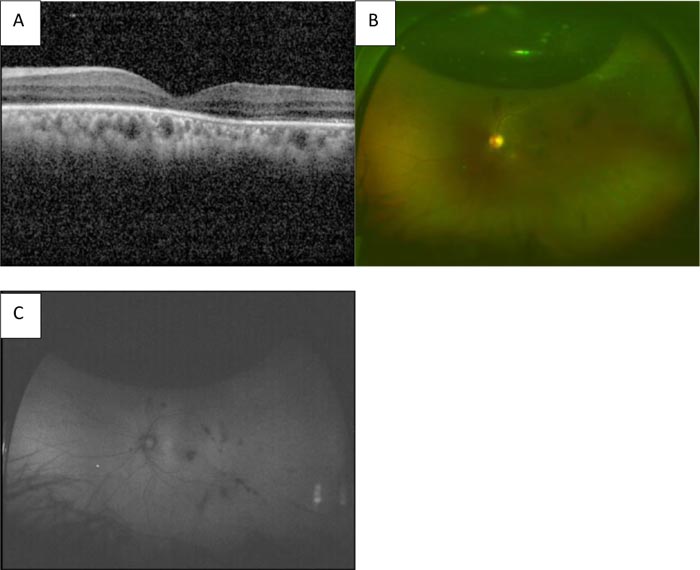
To reduce the time of contact and under full precautions, the patient underwent PR. The edges of the break were marked using high energy laser photocoagulation under the COVID-19 precautions (power:1000 milliwatts; size:microns; duration: 200 millisecond) then anterior chamber paracentesis of 0.3 CC was performed and 0.6 CC of pure sulfur hexafluoride- 6 (SF-6) gas was injected. The patient was instructed to perform the steamroller maneuver for 6 hours then maintain left side position. In the first visit, 3 days later, laser photocoagulation was done around the break with no complications. OCT showed resolution of Subretinal Fluid (SRF) with flat retina (Fig. 3A). On day 10 her vision improved to 20/40 in the affected eye. Wide-field color fundus photograph showed a flat retina (Fig. 3B).
2.2. Case 2
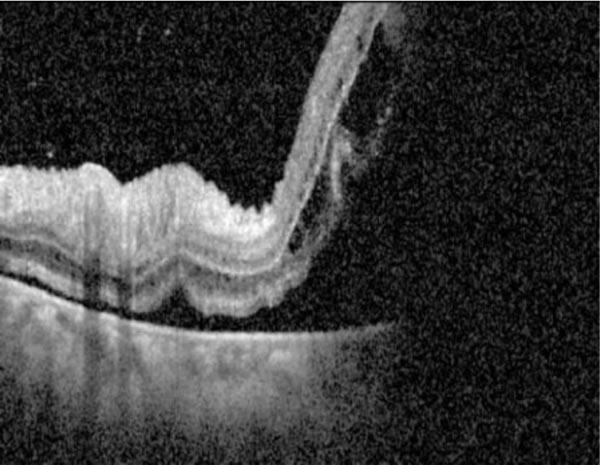
A 43 years old Saudi health care worker female confirmed COVID-19 case was presented to the emergency room at King Khalid Eye specialist Hospital (KKESH) with a history of flashes and floaters in the left eye, followed by painless vision loss 8 days before her presentation. No history of trauma was reported. She reported a history of complicated phacoemulsification with intraocular lens implantation OS 6 months earlier with posterior capsular rupture and vitreous loss. BCVA and Intraocular Pressure (IOP) at presentation of the left eye were 20/200, 11 mmHg OS respectively. Slit lamp microscopy revealed positive Shaffer sign, subtotal RRD with bullous configuration superior-temporally with a small horseshoe tear at 2 o’clock. Grade B Proliferative Vitreoretinopathy (PVR) was noted. Pre pneumatic retinopexy posterior OCT indicated detached macula (Fig. 4). Laser photocoagulation of the edge of the break was done to facilitate visualization after gas injection. Anterior chamber paracentesis of 0.2 CC was performed, and another 0.1 CC was aspirated after PR. Day 1 after PR the visual acuity improved with total resolution of subretinal fluid (Fig. 5). Subsequent laser was performed around the area of the break.
3. DISCUSSION
In ophthalmology, the proximity required of a thorough biomicroscopic slit-lamp examination and during surgery put ophthalmologists at increased risk of acquiring COVID-19 [6]. The Center for Disease Control (CDC) reported a decline in the Emergency Department (ED) visits in the United States by 42% from March 29th to April 25th. The Canadian Institute for Health Information (CIHI) noted that ED visits dropped by 25% in March 2020 compared with March 2019 [1]. Moorfield’s Eye Hospital estimates a drop in medical retina outpatient attendance to less than 30% of pre-COVID levels since lockdown began. Although, there is no exact data reported, similar reductions were observed in Saudi Arabia [7]. During COVID-19 pandemic, patients with primary RRD were more likely to delay in seeking treatment, present with macula-off RD, worse vision and PVR [3].
Exploring a quick and less invasive option in RRD management is essential to preserve vision and minimize the risk of infection. Arjmand et al. reported that PR was a commonly performed procedure during the pandemic with succusses rate of up to 72% [1]. PR is generally reported to be of superior to PPV in ETDRS visual outcomes in (months 3, 6 and 12) with less vertical distortion after 1 year of intervention [8].
Although anatomical success rate was higher in PPV compared to PR 93%, 81% respectively. The development of cataracts is much higher after PPV as 65% of patients required cataract surgery after one year while only 13% of patients post PR need intervention which can in turn reduce the burden of another procedure during the pandemic. Furthermore, PR was associated with better visual outcomes when compared to scleral buckle in macula off RD, which was notable in our cases [8].
CONCLUSION
PR represents an efficient and effective procedure in treating RRD and can be done in outpatient setup. Surgeons accustomed to the procedure can accomplish a higher success rate while needing fewer patient encounters. This can be valuable when measures of contact precautions are implemented, such as those encountered during COVID-19 pandemic.
ETHICAL APPROVAL AND CONSENT TO PARTICIPATE
The ethical approval for this study was obtained from Research Ethics Committee of King Khalid Eye Specialist Hospital (Reference No. RD/26001/IRB/0155-2).
HUMAN AND ANIMAL RIGHTS
Not applicable.
CONSENT FOR PUBLICATION
Written and informed consent from the patients was obtained for publishing this case report.
STANDARDS OF REPORTING
CARE guidelines were followed in this study.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


