Impact of Lifestyle Management on COVID-19
Abstract
Background:
The Coronavirus Disease 2019 (COVID-19) is a highly contagious and deadly viral infection that led to a pandemic situation and has become the biggest challenge to overcome since its inception. To date, many infected people have lost their lives and many are suffering a lot due to post-COVID complications. The corona outbreak imposed different countries to undergo lockdown, which resulted in huge economic losses. The world is again battling with a new variant of Corona ‘Omicron’, which is spreading even more. Few reports have indicated that vaccinated people are also getting the infection and in some cases of new variants, serious complications are also observed. Scientists are yet striving to come forward with time-tested and registered medicines to eradicate the infection.
Objective:
A healthy lifestyle incorporating good food habits, ample physical activity, cessation of addictions, self-hygiene, and enough sleep to reduce stress and anxiety can help people in generating strong immunity. The objective of this review is to spread awareness among people regarding the significant role of lifestyle management in the development of strong immunity against COVID-19.
Methods:
All the information regarding different aspects of lifestyle management and COVID-19 was gathered through an exhaustive literature survey of books and scientific resources.
Conclusion:
The mortality and severity in the cases of COVID are many-a-times associated with low immunity. The virus is also getting mutated and may override the vaccine’s effectiveness. Hence, strong immunity plays a key role in supporting people, especially those with co-morbid health conditions, for the prevention of COVID-19 and that can be achieved by maintaining a healthy lifestyle.
1. INTRODUCTION
Immunity is a basic weapon to fight any infection. The world’s battle with Severe Acute Respiratory Syndrome Corona Virus 2 (SARS-CoV-2) has taught us many lessons that include the value of a healthy lifestyle and the significance of developing good immunity. We have witnessed that symptoms and severity of COVID-19 infection vary in the infected people. Some people remain asymptomatic, while others show mild to severe symptoms, sometimes leading to complications or death. This variation occurs due to the difference in the immune responses of the host body. Hence, immunity plays a major role in the prevention of infections, particularly in cases of pandemic situation. Strengthening the immunity does not assure the people that they will not encounter the COVID infection, but the severity can be controlled by maintaining immunity. It is suggested by health practitioners that a healthy and nutritional diet along with adequate physical activity can help to build up natural immunity in order to fight the disease, even after getting infected [1-3]. Since the COVID-19 pandemic outbreak, people have started undertaking health measures like personal isolation, wearing face masks, social distancing, sanitization, frequent hand washing with soap and running water, avoiding touching the face, eyes, nose, mouth, and vaccination [4]. For the treatment of COVID-19 infection of mild impact, medical practitioners prescribe drugs like hydroxychloroquine, favipiravir, ivermectin, azithromycin, dexamethasone, and methylprednisolone during home isolation [5]. Despite this, some people develop severe symptoms and need to be hospitalized due to a decline in blood oxygen levels as soon as the virus invades the lungs. Additionally, the patients with co-morbidity are at higher risk of developing complications. These co-morbidities include hypertension, diabetes, coronary artery disease, and other diseases, most of which fall under lifestyle disorders. Once infected by the Coronavirus, the recovery depends mainly on the host immune system, which plays a crucial role in the management and eradication of COVID-19 [6]. The immune system fights the infection by generating antibodies. However, the elimination of infection must take place at the appropriate time i.e. before it spreads and damages other organs. Undoubtedly, COVID-19 outbreak has made people realize the importance of effective immunity that can be achieved through a managed healthy lifestyle [7].
Last year during April and May, people across the world have witnessed a resurgence of COVID-19 cases and are still striving to resume their normal lives. Hence, it is the need of the hour to highlight the significance of lifestyle management in strengthening the innate immunity [6]. A healthy lifestyle, including a balanced diet carrying the required amounts of macronutrients and micronutrients, is a prerequisite for the optimized immunity. On the other hand, unhealthy habits like the consumption of alcohol and tobacco may lead to a compromised immune system. As obesity is one of the risk factors leading to co-morbidities in COVID-19, the maintenance of body weight in accordance with the Body Mass Index (BMI) serves as an important preventative measure. Furthermore, adequate functioning of the immune system requires sufficient restorative sleep, regular exercising, regular practicing of yoga, and meditation along with timely vaccination [7]. The lifestyle factors are described in Fig. (1).
People must also realize the importance of vaccination in the development of immunity against COVID-19. Vaccines are made up of inactive parts or weakened parts of a particular virus or other organisms (antigen) that stimulate the immune system. This weakened version is not able to produce the disease in the body, but it will prompt the immune system to respond as it would be its first response to the actual virus or organism. Different types of vaccines have different mechanisms to generate such protection. But in the end, the immune response generates ‘memory’ T-lymphocytes and B-lymphocytes, which are now trained to fight the virus. This process of generating B-lymphocytes and T-lymphocytes in the body after vaccination requires a few weeks. Thus vaccine requires enough time to provide protection and the person may catch the COVID infection before or just after the vaccination. During the process of immunization, some people may develop common symptoms, such as fever, pain, and discomfort. Many people have reported allergic reactions to the vaccines and an occurrence of blood clots after the administration of some COVID-19 vaccines [8].
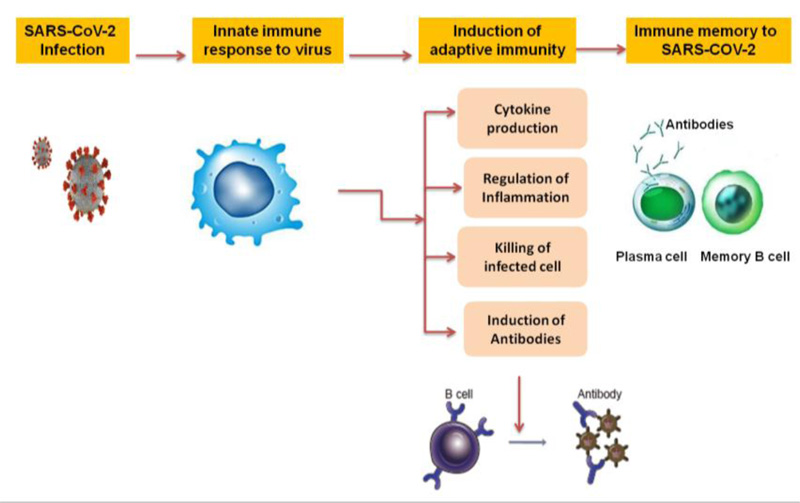
2. IMMUNITY
To combat any bacterial or viral infection, the human immune system acts mainly in two ways, as shown in Fig. (2). The first approach is through innate immunity or inherited immunity. The innate immune system is featured with a rapid response to infection as soon as it enters into the body, resulting in the generation of inflammation and fever. It does not recognize any specific strains of bacteria or viruses and that is why it is unable to get rid of all the pathogens. The second approach is through acquired or adaptive immunity. In this case, during the first exposure to the germs, the immune system tries to fight the infection, and symptoms of the infection occur. However, the immune system remembers the specific invader and enables the body to fight it strongly on consecutive exposures [9, 10].

2.1. Key Players of the Immune System
Frontline active players in our immune system are the white blood cells, also called leukocytes. Leukocytes are activated innate immune cells, which circulate throughout the body and search for intruders. When a foreign substance is detected, they stimulate the sequence of responses to combat the invader [ 9, 10]. Leukocytes can be converted to phagocytes (macrophages) and lymphocytes. Phagocytes engulf the foreign infectious agent and break them down, resulting in the generation of the Cytokines and symptoms of inflammation, like fever and pain [10]. On the other hand, lymphocytes are of two types, B lymphocytes (or B-cells) and T lymphocytes (or T-cells). Out of these, the B-cells create antibodies to shatter the pathogens, whereas the T-cells are further of two types, CD4 (Cluster of differentiation 4), and CD8 (Cluster of differentiation 8). The CD4 and B-cell lead to resistance against infections, while the CD8 cells can produce a cytotoxic effect on invader cells [11, 12].
3. LIFESTYLE FACTORS AFFECTING IMMUNITY
3.1. Food Habits
Immunity is directly associated with the nutrition of food and sufficient hydration in people of all age groups [12]. Adequate energy supply is needed by immune system cells to respond to infection effectively. During the periods of infection, the ‘activated’ immune system requires a further supply of energy, with higher basal energy expenditure during fever [13]. A protein-rich diet is required to generate quality immune proteins such as cytokines and immunoglobulins [14]. In contrast, a carbohydrate-rich diet should be avoided specifically in diabetic patients. A high sugar diet is also associated with an increase in complications and severity of COVID-19 infection [15].
Especially in cases of heavy viral load, Vitamin C plays a significant role in dealing with high oxidative stress [16, 17]. Additionally, vitamin E is an inhibitor of protein kinase C activity [18]. Some minerals like zinc, iron, and magnesium need to be consumed in adequate amounts for nucleic acid synthesis for immune cells, while vitamin C and vitamin E owing to their antioxidant effects, protect the tissues from damage by viral infection [19]. Vitamin D-rich food is also essential for protective action on the respiratory system [20].
It is a common observation that people take medicines, mainly dietary supplements, on their own without consulting the doctors. Especially since the COVID-19 pandemic, people have started gulping many supplements to boost their immunity. Some of the supplements may improve general health if taken in the proper amount, but others may be harmful or ineffective. For example, studies have reported that a daily dose of more than one gram of calcium can increase the risk of death from cancer [ 21 ]. It has also been shown that adequate amounts of vitamins A, vitamin K, zinc, and magnesium may lower the risk of death, provided those nutrients are acquired from food and not from supplements. Similarly, Vitamin D supplements can harm kidneys, if taken frequently in large quantities. A blood level of vitamin D higher than 100 nanograms per milliliter (ng/mL) can stimulate extra calcium absorption, causing mood disorders, muscle pain, abdominal pain, kidney stones, heart attack, and stroke. Protein is also one of the important nutrients, which uplift the general health and thereby the immunity. However, over-consumption of protein for a prolonged period must be avoided, as it may increase the metabolic burden on the kidneys and liver, simultaneously potentiating the risk of cancer and heart diseases [22].
Consumption of a nutrient-poor diet, especially deficient in protein, leads to malnutrition, eventually leading to a state of poor immunity and may result in a higher risk of getting the COVID-19 infection [ 21 ]. People who take a balanced and healthy diet have stronger immunity as compared to people who consume junk and frozen food [22]. Furthermore, over-eating and unhealthy diets containing high fats and carbohydrates may be associated with fat-deposition. This results in the generation of constant systemic inflammation of low grade due to discordance of the immune system, thereby increasing the severity of COVID-19 infection [23].
3.2. Obesity
Subjects with severe obesity (Body Mass Index ≥ 40 kg/m2) are at a higher risk for COVID-19 infection as well as its complications [24]. As discussed earlier, having a correct nutritional balance is crucial, especially amidst the pandemic when the immune system should be ready to fight and combat the infection at any time. Overeating habits and craving for a high sugar diet may threaten the health of people. There are many incidences suggesting that the generation of cytokinesis is higher in extended adipose tissues with high content of lipid, leading to elevation of unwanted inflammation [25]. Obese people have decreased expiratory reserve volume, respiratory system compliance, and functional capacity and hence it becomes difficult for them to survive the COVID-19 infection. In severe cases of coronavirus infection, ventilation would be more difficult in the obese subject, even in the supine position as their pulmonary function is compromised by decreased diaphragmatic excursion [26]. The inflammatory state characteristics of obesity could further exacerbate the inflammation in patients with COVID-19, thus exposing them to a higher concentration of proinflammatory cytokines, making them prone to the threat of a ‘Cytokine storm’ [27-29].
3.3. Physical Activity
Physical exercises reduce anxiety, decrease the risk of depression improve the quality of sleep, and give a sense of psychological wellbeing [30]. The immune system is also improved by moderate exercise and physical activity. A daily physical exercise of less than 60 minutes activates anti-pathogen effects of tissue macrophages and enhances recirculation of neutrophils, cytotoxic T cells, immunoglobulins, NK cells, anti-inflammatory cytokines, and CD8+ T lymphocytes which synonymously boost the immunity. Acute improvement in the level of Interleukin (IL-6) levels also occurs with moderate exercise, which in turn produces direct anti-inflammatory effects and eventually elevates the metabolism of glucose and lipid. Regular physical activity may also correct co-morbid complications that will minimize the risk of severity of COVID-19 [31, 32]. Reports have suggested that people undertaking inadequate physical activity are more prone to COVID-19 infection as compared to physically active people and the chances of their hospitalization and severe complications are also more. Physical inactivity is also a key risk factor for cardiovascular diseases, cancer, and diabetes which has led to death during the COVID-19 pandemic worldwide [33]. However, prolonged vigorous exercise for a long duration may result in metabolic, psychological, and physiological stress leading to immune dysfunction. Hence, such vigorous exercises should not be suggested for people at high-risk or with suspected and confirmed COVID-19 cases. It can also increase the oxidative stress on the lungs and heart and hence it is recommended to avoid such exercises in the patients who recently recovered from corona and had moderate to severe symptoms while infected [34].
3.4. Use of Tobacco and Drug Abuse
In addition to several injurious effects of smoking on different organ systems of the human body, smoking is also likely to induce severe coronavirus disease [35]. Confirmed COVID-19 cases who smoked tobacco are more likely to suffer from moderate to severe symptoms as compared to non-smokers [36]. Tobacco smoking also leads to poor prognosis and mortality in infected individuals. According to available medical information, exposure to tobacco and other addictive substances (like methamphetamine, opioids, and cannabis) promotes the release of pro-inflammatory cells that causes high damage to the body, particularly the lungs [37]. Such individuals are at a higher risk of developing Severe Acute Respiratory Distress Syndrome as compared to non-addictive people [38]. There is a great elevation in the chances of catching the infection from bacteria like Haemophilus influenza, Streptococcus pneumoniae, Legionella pneumophila, and Neisseria meningitidis, particularly affecting the lungs, in adult smokers and this explains the reason behind the huge occurrence of secondary bacterial infections in smokers who get infected with COVID-19 [39]. Research findings have clearly indicated 14 times higher incidences of severe pneumonia as well as stage III COVID-19 infection and eventually death in smoking-habituated people as compared to those with no smoking habits [40].
The immune function of the nasal cavity decreases on habitual tobacco inhalation by compromising the mucociliary clearance of foreign bodies. The expression of genes for the immune system is also altered in smokers and drug addicts, including genes involved in inflammation [41]. Studies have suggested a positive correlation between quitting tobacco and improved clinical outcome during COVID infection, especially with co-morbid conditions (like Diabetes Mellitus and cardiovascular diseases), which in turn results in a better prognosis [42].
Similarly, over-consumption of alcohol has also been shown to reduce immunity, cause poor prognosis during COVID-19 management and increase the risk of Acute Respiratory Distress Syndrome and other complications [43, 44].
3.5. Sleep
Sleep is an essential physiological process and taking enough sleep of at least 7 hours per day is desirable to maintain good immunity, especially against infections of viral origin [45]. Alteration in sleep cycle or lack of sleep particularly rapid eye movement (REM) sleep alters the components of the immune system, such as the percentage of the immune cell sub-populations like CD4+, CD8+, and NK (Natural killer) cells and cytokine levels like IFNγ (Interferon-γ), TNFα (Tumor Necrosis Factor-α), and IL-1(Interleukin-1)), which in turn increases the risk of contracting COVID-19 and also delays the recovery from it [46, 47]. Findings have suggested that in COVID-19 infected patients, sleep deprivations may result in elevation of CXCL9 (Chemokine C-X-C motifligand 9) levels which is a chemotactic factor that selectively causes lymphocytic infiltration and activation of pro-inflammatory NLRP3 (NLR family pyrin domain containing 3) inflammasome. Hence, sleep deprivation may be responsible for increasing the severity of infection due to the enhancement of the progression of inflammatory processes [48].
Deep and adequate sleep is also reported to increase the level of melatonin, a hormone that improves sleep quality and also possesses anti-inflammatory properties. Adequate sleep can reduce coronavirus virulence by reducing the inflammatory response and thus offer protection to the lungs from oxidative damage [49, 50].
3.6. Stress
Since the start of the COVID-19 pandemic, many people are facing challenges not just due to COVID-related health issues, but also due to other factors like fear of infection, emotional disturbances, social isolation, and financial insecurities. The prevailing conditions are stressful as people are enforced to follow the strict regulations for the prevention of the spread of viral infection and simultaneously they are also managing their life to meet daily financial requirements. Such stress can be harmful to the body in many ways [51]. It can decrease the body’s ability to react to different diseases [52]. Chronic stress may result in many lifelong stress-induced diseases such as insomnia, gastric ulcer, coronary artery disease, and type 2 diabetes mellitus. Stress can also reduce immunity and induce the release of hormones such as cortisol and adrenaline that are associated with disrupted immune regulation and elevation in proinflammatory cytokine (IL-6) levels [53]. Prolonged mental stress can also amplify the levels of histamine further worsening acute respiratory distress syndrome and increasing the severity of COVID-19 infection [54, 55].
According to a study aimed at psychological evaluation of COVID-19 infected patients admitted in isolation wards, about 48% of patients demonstrated psychological stress. This elevated stress thereby led to a slow recovery or increased severity of the infection [56].
Additionally, it was recorded that the long duration of hospital stays and the isolation fear increased the psychological stress in patients to such an extent that it manifested into anxiety disorders and eventually exacerbated panic attacks, specifically in the case of patients with a history of pre-existing psychological disorders [15]. In such cases, the patient compliance in the management of COVID-19 gets compromised, thereby affecting the outcome of treatment. Therefore, stress management strategies are highly recommended for individuals, suspected, and confirmed cases, families, and health professionals, in the pandemic situation. Regular and mild aerobic exercises, meditation, yoga, guided imagery, and breathing and relaxation techniques can help in reducing stress and also in maintaining sleep quality thereby boosting immunity and confidence. Managing a healthy lifestyle, positive psychology, strengthening social connections, and healthy relationships with loved ones are the main pillars in the strategy of stress management during this pandemic area [56].
3.7. Self-hygiene
According to health professionals, the best and simplest ways to prevent the spread of COVID-19 is by washing hands frequently, covering the mouth and nose with a mask while coughing and sneezing as well as avoiding frequent touching of the face [57]. Face touching can allow germs to enter the body through the eyes, nose, and mouth therefore it becomes mandatory to avoid it. The mouth and nose should be covered with an elbow while sneezing or coughing and tissue paper should be disposed of immediately off [58]. Every individual should cover their mouth and nose with a mask while going outside or in public. Reusable masks must be washed daily with soap or detergent and disposable masks should be cut into two parts before disposing of them to avoid reuse [59].
Home cleanliness is equally important to avoid the spread of the pandemic. Hence, care must be taken to make the living spaces free from viruses. Highly used surfaces should be cleaned and disinfected frequently. Before using the disinfection products, the specifications of the product should be read properly as some disinfectants need to have sufficient contact time with germs and viruses to kill them. As per the medical guidelines, the COVID-19 virus can also survive on fabric as well as on plastic and metal elements and it may live for longer times from hours to a few days. Moreover, other good-hygiene practices like removing shoes, changing the clothes, and proper sanitization before entering the home are prerequisites to prevent the entry of viruses at home [60].
3.8. Phytomedicines
During the last few years, the inclination of people toward using phytonutrients and phytomedicines has increased to improve immune health and also alleviate the symptoms associated with COVID-19 infection. Various herbal extracts and formulations including traditional medicines are also being used for the prevention and complementary treatment of viral diseases, including COVID-19 and other respiratory tract infections. Various traditional herbs, especially Tinospora, Ashwagandha, Curcuma, Ocimum, are either consumed in raw form or modified into decoctions for immunomodulator effects. Although complete clinical data is yet lacking to confirm the efficacy of these herbal preparations, phytochemicals have shown promising results based on their mode of action. Phytochemicals that have been acknowledged as effective immunity boosters include polyphenols, especially flavonoids. Flavonoids like kaempferol, quercetin, and apigenin represent a class of phytochemicals that are acknowledged to possess antiviral activities in various in silico studies [61, 62].
As phytochemicals have demonstrated potential therapeutic effects against viral infections, including COVID-19, they can be regarded as a good source of alternative and cheaper medicines. They may also be incorporated into the lifestyle as health supplements or as an adjuvant for boosting general immunity as well as for prevention or treatment of COVID-19 infection. However, some important limitations in the use of phytomedicines include the lack of quality parameters and insufficient evidence of the protective and therapeutic effects in humans along with a lack of bioavailability, pharmacokinetic, and toxicological studies of these phytomedicines [62].
3.9. Vaccination
It is proven that in case of any pandemic, including a coronavirus outbreak, vaccination is the most promising remedy that works on the concept of strengthening immunity. On exposure to the first dose of the vaccine, our body starts to produce antibodies against COVID-19 that in turn enables the immune system to fight the virus whenever it enters the body encounters, thereby reducing the chances of getting infected by the disease [63].
| Name of the COVID-19 Vaccine | Place of its Origin | Type of the Vaccine | Percentage of the Protective Effect |
|---|---|---|---|
| Corbevax vaccine | California | Protein subunit made up of SARS-CoV-2 protein | 95% |
| Covaxin | India | A whole inactivated virus-based COVID-19 vaccine | 81% |
| Covishield | United Kingdom and India | Non-replicating viral vector vaccine | 70.82% |
| Janssen vaccine | Netherlands and Belgium | Non-replicating viral vector vaccine | 66% |
| Moderna vaccine | United States | mRNA-based vaccine | 94% |
| Novavax vaccine | United States | Protein subunit made up of SARS-CoV-2 protein | 89% |
| Sputnik V vaccine | Russia | An adenovirus viral vector vaccine | 92% |
| Pfizer-BioNTech vaccine | America | mRNA-based vaccine | 95% |
Herd immunity is generated by vaccination of a maximum number of people that minimizes the chances of infection as well as the spread of the virus. Apart from self-safety practices, vaccinated people also reduce the transmission of the virus thus helping society as well as countries in such pandemic situations. In addition, a new study has suggested that if an expectant mother has taken the vaccine, the produced antibody can cross the placenta and can enter the unborn baby providing it the passive immunity. Vaccinated-feeding mothers can also protect their babies by breastfeeding as breast milk carries the antibodies against COVID-19 [64].
However, as per the reports of the Center for Disease Control and Prevention (CDC), vaccines remain effective in protecting most people from COVID-19 infection and its complications but the vaccine may not be 100% effective. Thus, vaccine breakthrough infections may occur when a fully vaccinated person gets infected with COVID-19 and the people with vaccine breakthrough infections may spread COVID-19 to others. In the case of immunocompromised people, adequate levels of protection are not achieved even after the administration of the two-dose primary mRNA COVID-19 vaccine. Thus, CDC advises that people should continue taking all the precautions recommended for unvaccinated people and also receive an additional booster dose of the vaccine [65]. The vaccines used for immunization against COVID-19 infection are enlisted in Table 1. Out of all the vaccines, Covishield and Covaxin are more prevalent in India [66].
Looking to the safety concern, it would be far more useful if people strive to develop strong immunity on daily basis by following a healthy lifestyle.
CONCLUSION
Since January-2019, the COVID-19 pandemic has affected people worldwide. Even today, many countries are battling against the deadly virus and the spread of this disease has not ceased yet. The healthcare professionals are also getting affected while treating the COVID-19 infected patients even though they are taking all the precautions. The virus is mutating and new mutants are more contagious and pathogenic. The world has again entered a new alarming situation as a new variant of Corona ‘Omicron’ is spreading in many countries rapidly. The best medicine to treat this disease is yet to be discovered and mutants have posed a big challenge to the world. A strong immune system can help people deal with this pandemic. Immunity is our only weapon to win this battle and to make the world free from COVID-19. A healthy lifestyle helps to build strong immunity and hence the focus of the population should shift to lifestyle management. The objective of this article is to make people aware of various lifestyle factors that may help to develop and enhance immunity i.e. healthy diet, regular exercises, yoga, cessation of addictive product consumption including tobacco, and taking adequate rest and quality sleep to reduce psychological stress. People with co-morbidities should be guided about risk factors associated with COVID-19 as they are more vulnerable. Lifestyle management controls disease progression, prevents the severity of disease, and shortens the post-COVID-19 recovery time. However, vaccination against COVID-19 is also crucial for the prevention of this disease. During the third wave of COVID-19 especially of the Omicron variant, it was observed that people who were vaccinated experienced only mild flu-like symptoms also recovered faster as compared to the non-immunized people. Hence, it is recommended that lifestyle interventions along with vaccination should be a part of the COVID-19 management protocol until the world can get an effective magic bullet as its remedy. This would contribute to regaining normal lives soon as people would have high immunity to fight the COVID-19 infection and also downgrade the spread of this infection.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| REM | = Rapid Eye Movement |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial, or otherwise.
ACKNOWLEDGEMENTS
The authors are thankful to L. M. College of Pharmacy, Ahmedabad, Gujarat, India for providing the necessary facilities for the literature survey and access to online resources to gather comprehensive information for the review article.