Long COVID Symptoms in the ENT: Coordinating Community and Hospital Services in the United Kingdom
Abstract
The COVID-19 pandemic has had a catastrophic effect on the entire world, and the WHO has described it as the worst global health emergency it has ever faced. A highly significant positive development was the relatively quick creation of safe and effective vaccines, but persistent problems like the appearance of variants that are highly contagious have complicated the plans for ending the pandemic. It is now a widely acknowledged fact that a sizable number of people who are infected will suffer for a long time from a complicated and potentially crippling chronic sickness, the so-called “Long COVID”. A significant portion of COVID-19 patients who experience ENT symptoms do not entirely recover from these symptoms. This article will discuss the ENT manifestations of COVID-19 along with their prevalence, pathogenesis, natural course, persistence in some individuals, and contribution to Long COVID-19. Also, it will go over broad guidelines and principles for treating patients with Long COVID as a whole, followed by a more detailed discussion of how ENT services in the UK could be set up in a way that is safe, efficient, and ensures that the workforce is utilised as effectively as possible.
1. INTRODUCTION
The COVID-19 pandemic started with a small number of fatal novel human pneumonia cases in Wuhan, China, towards the end of December 2019. This was the start of the first known coronavirus pandemic in history and the sixth verified pandemic since the 1918 flu pandemic [1]. The WHO temporarily called the virus the 2019 novel Coronavirus (2019 CoV) and next formally named the disease Coronavirus Disease 2019 (COVID-19). Following this, the virus was officially named Severe Acute Respiratory Syndrome Coronavirus -2 or SARS-CoV-2 [1, 2]. This highly contagious disease rapidly spread worldwide and had a devastating impact globally.
There is a broad and diverse spectrum of clinical symptoms associated with SARS-CoV-2 infection, from asymptomatic and moderate cases to severe disease with multiorgan failure [3, 4]. While the basic symptoms, which predominantly affect the lower respiratory tract and include fever, cough, and dyspnea, have been gradually recognised during the pandemic, there are a number of extrapulmonary presentations.
Of these, ENT symptoms have been found to be extremely prevalent. The first ENT symptom of SARS-CoV-2 was olfactory dysfunction (OD) with or without loss of taste [4, 5]. The prevalence rates that were published varied greatly. According to a meta-analysis of 27 studies [6], the estimated global pooled prevalence of loss of smell among moderate and severe COVID-19 patients was 48.47%, that of loss of taste was 41.47%, and that of both was experienced by about 35% of patients. In 11.8% to 27% of individuals, OD has been reported to be the first symptom of COVID-19 [7].
Otolaryngologic symptoms comprise a large proportion of mild COVID-19 symptomatology, with reports of smell and taste disturbance being the only manifestation in “asymptomatic” individuals. Therefore, OD and/or loss of taste are now considered cardinal symptoms of COVID-19 [8]. The other common ENT symptoms included sore throat and rhinorrhoea. Several other less common and atypical ENT manifestations have also been reported to be associated with COVID-19. These include acute otitis media, SNHL etc. [9].
According to reports, the prevalence of anosmia or dysgeusia is noticeably lower among Asian people. According to an Indian prospective study [10], the overall incidence was barely 20%.
2. NEUROPATHOLOGIC BASIS
The mechanism for post-viral olfactory dysfunction, including that from COVID-19, is highly complex and virus-dependent and could occur due to insults at multiple levels of the olfactory pathway [11].
The primary entrance point for SARS-CoV-2 is the olfactory epithelium, where the virus is known to connect to ACE-2 receptors. The fact that the majority of COVID-19 patients who experience loss of smell eventually regain olfactory function may be explained by the fact that the genes encoding the ACE2 receptors are only co-expressed by a small subset of sustentacular cells, horizontal basal cells, and Bowman's gland cells (and not the olfactory nerve bodies themselves) [11-14].
According to the “Two Hit Hypothesis,” synaptic plasticity should be impaired in order for post-viral OD to persist in addition to the initial viral damages [11].
According to Dias de Melo et al., long-lasting COVID-19-associated anosmia patients' olfactory mucosa samples showed the presence of virus transcripts and SARS-CoV-2-infected cells as well as persistent inflammation [8].
There have been further hypotheses. According to Addison et al. [15], a bigger region of the olfactory epithelium being impacted by the coronavirus may be the cause of the persistence of olfactory dysfunction.
3. RECOVERY AND PERSISTENCE
Despite the fact that the majority of COVID-19 patients will naturally regain their sense of taste and smell, a sizable portion of them will not regain it and experience long-lasting sensory changes [14].
In their group of 145 patients, Panda et al. [10] observed that 96% of the patients had fully healed after 4 weeks. However, this study was conducted in India, where the prevalence of OD was also much lower than the average worldwide.
According to other studies, 10%–17% of COVID-19 patients will still have OD and not recover on their own [15]. After a 6-month follow-up, Kapoor et al. reported a prevalence of persistent OD of 12% [16].
4. LONG-COVID AND ITS EFFECTS ON THE WORLD:
Late in the clinical course of COVID-19, symptom persistence or the emergence of new symptoms is a significant issue that the infected population around the world and their healthcare systems are dealing with [17, 18]. The phrases “Long COVID” or “Covid Long Haulers” are frequently used.
In May 2020, Italian patient Elisa Perego coined the phrase “Long COVID-19” as a hashtag on Twitter to describe her own experience of having symptoms long after COVID-19 recovery [19].
About 10% of COVID-19 survivors are thought to still have symptoms weeks or months after the onset of the initial symptoms [20]. According to the Office of National Statistics, one in ten people experience symptoms for at least 12 weeks [21]. Although a number of risk factors have been found (some of which are listed here), it is crucial to remember that young, previously healthy people who have mild disease are also thought to be at risk [22].
In a prospective cohort research involving 312 patients, Blomberg et al. found that 61% of patients still had symptoms after 6 months [23].
5. NAME AND DEFINITIONS
The National Institute of Clinical Excellence (NICE) in the UK uses the following clinical definitions for the initial sickness and extended Covid in its December 2020 recommendation [24].
Acute COVID-19: Signs and symptoms of COVID-19 for up to 4 weeks.
Ongoing symptomatic COVID-19: Signs and symptoms of COVID-19 from 4 to 12 weeks.
Post-COVID-19 Syndrome: Signs and symptoms that develop during or after an infection consistent with COVID-19 continue for more than 12 weeks and are not explained by an alternative diagnosis.
In addition to the clinical case definitions, 'long COVID' is commonly used to describe signs and symptoms that continue or develop after acute COVID-19. It includes both ongoing symptomatic COVID-19 and post-COVID-19 syndrome.
6. RISK FACTORS
The following are a few of the known risk factors for Long COVID development [22, 25]. Further investigation is required into these.
• Female sex
• Older individuals
• Pre-existing medical conditions
• Those who required hospitalisation
• More than 5 early symptoms
• Early dyspnoea
• Prior psychiatric disorders
• Specific biomarkers like D-Dimer and CRP
7. ENT SIGNS AND SYMPTOMS OF LONG COVID
With a reported incidence of 12% at 6 months, persistent OD is the second-most prevalent Long COVID symptom [16]. People with anosmia are more susceptible to possible risks from things like contaminated food and gas, which can have a major emotional impact. Physical difficulties may also result from a decreased appetite brought on by a loss of enjoyment from eating [26].
It is possible that some cases of persistent OD go unreported. Just 50% of patients with persistent hyposmia acknowledged their ongoing impairment in olfactory discrimination and identification, according to objective assessments [29].
Long covid is also said to cause parosmia and phantosmia. Some of the regenerated neurons may be “misguided,” according to the neuropathological explanation for parosmia, and end up in aberrant regions of the brain [27].
According to some theories, paradoxical vocal fold movement problems caused by Vagus nerve irritation may be the cause of recurrent shortness of breath in some Long Covid patients, necessitating ENT evaluation [14].
Patients with severe Covid may also experience laryngotracheal stenosis brought on by tracheostomy or prolonged endotracheal intubation [28].
7.1. Treatment of Olfactory Dysfunction in Long COVID Patients
As previously said, OD can result in serious morbidity, such as dietary issues, social anxiety, and depression [15].
While treating OD, educating, involving, and empowering patients is critical. Patient education pamphlets [29, 30] and other tools are crucial for enhancing patients' comprehension.
Metanalyses and numerous prospective controlled studies provide compelling evidence that Olfactory Training (OT) helps people with OD improve their olfactory function. After 12 or more weeks of therapy, the traditional OT, which entails exposing patients to 4 different odorants for 5 minutes each, has been found to improve olfactory function [15].
Altundag et al. [31] compared the traditional OT with 4 odours over a 36-week period to a modified OT utilising 12 odours. In the 12 odour group, odours were changed every 12 weeks. They have reported better results compared to classic OT [16].
A flowchart of secondary care therapy options was recommended in a worldwide Clinical Olfactory Working Group consensus statement on Post Infectious Olfactory Dysfunction [15]. OT was reaffirmed as the backbone among the different solutions mentioned, with a few additional management possibilities.
The BRS consensus guidelines on the management of new-onset anosmia in the COVID-19 pandemic [32] outline the following.
1. OT is recommended for patients with OD more than 2 weeks
2. Patient support in the form of advice and direction to AbScent and Fifth Sense was recommended.
3. Intranasal corticosteroid sprays were recommended for OD more than 2 weeks with nasal symptoms.
4. Intranasal corticosteroid drops or rinses were optional to recommend in patients with OD more than 2 weeks associated with nasal symptoms.
5. Oral steroids were not recommended for patients with OD more than 2 weeks with persistent COVID symptoms. They were optional to recommend in a patient with OD for more than 2 weeks when that was the only remaining symptom.
6. No recommendation could be made on Vitamin A drops
7. Alpha Lipoic acid was not recommended, and Omega 3 supplements were optional for patients with this as an isolated symptom.
7.2. Long COVID Service Design Considerations: Looking out for the Long haulers
Since March, the ONS (Office of National Statistics) estimates have indicated that about a million people in the UK have reported experiencing Long Covid-related symptoms. The most recent projection was 962,000 (1.5% of the population) as of June 6, 2021 [33].
According to a news release from the Department of Health and Social Care on June 24, 2021, 2 million people in England may have developed Long Covid, based on the results of the REACT-2 study. This was 5.8% of the study participants, and 2% of them reported having severe symptoms [34].
Long COVID symptoms can be many, multisystemic, and variable over an extended period of time. Every Long COVID consultation should make sure that the patient's symptoms are openly acknowledged and that there is honest dialogue. Patients should have continuous access to multidisciplinary treatments, such as telehealth and rehabilitation [35].
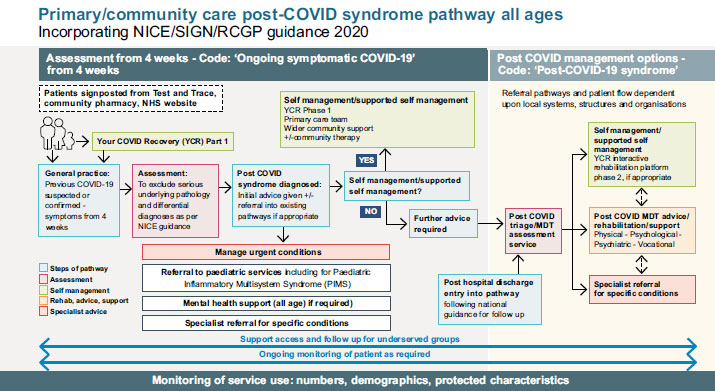
Version 2 of the National Guidelines for Post-COVID Syndrome Assessment Clinics was released by NHS England and Improvement in April 2021 [36]. This update was made when the NICE, the SIGN, and the RCGP released the COVID-19 fast guideline: managing the long-term consequences of COVID-19 [18, 36]. This publication, among other things, identifies a distinct clinical route (Fig. 1).
8. CONSIDERATIONS FOR ENT SERVICES
Based on the established prevalence rates, it is anticipated that a sizeable portion of the population may experience persistent OD after receiving a confirmed or suspected diagnosis of COVID-19.
The organisation of ENT services must take into account the broader context of managing Long COVID because many of these patients may also be experiencing other Long COVID symptoms. The NHS E&I advice [36], as stated, states that the location of service delivery is left up to local discretion and may be situated in primary, secondary, or community services as long as fast access to suitable diagnoses and treatments is available. The services should also include a virtual component.
The NHS England document Transforming Elective Care Services: Ear, Nose and Throat [37], in a section titled National ENT Challenge, points out that in the year 2017/18, GPs made nearly 900,000 ENT referrals in England alone, accounting for nearly 7.6% of all referrals to secondary care. It also highlights the lack of capacity in secondary care, the need for multidisciplinary work with primary care, and the need to support patients in managing their condition in the community using patient education and information resources.
These principles have become much more important now in the face of new challenges due to a substantial increase in the percentage of the population suffering from OD.
In this situation, it is anticipated that service delivery plans for OD related to Long COVID will be created with a focus on primary care. As a result, Physicians are expected to experience a significant increase in OD patients. To deal with these patients both mentally and physically, they need to be given enough resources and assistance [26].
Essentially, these patients are likely to be managed by GPs with Olfactory Training carried out in the community by patients themselves with the appropriate information, advice, and support, with the exception of referral to ENT services in situations like red flags, specific alternative diagnoses, or failure to improve. Patients should be directed to these as soon as feasible. The majority of this help might be found on websites like Fifth Sense and AbScent.
Apart from key instances in the algorithm where face-to-face interactions are essential, it is possible for other consultations, especially follow-ups during an expected course, to be carried out virtually both in primary care and secondary care.
It is essential that the service delivery and referral pathways for the management of persistent OD (and the other rarer ENT symptoms of Long Covid) in primary care/community fit into the holistic and person-centred approach to dealing with Long Covid patients. As the NHS E&I guidance [15] suggests, integrated referral pathways between primary and community care, multidisciplinary rehabilitation and specialist services, multidisciplinary assessment clinics, and specialist mental health services should be agreed upon. Moreover, the pathways for the management of persistent OD and other ENT symptoms should fit into these pathways.
CONCLUSION
The COVID-19 pandemic still has a significant disruptive effect on the world economy due to the appearance of new strains and other causes, despite the quick discovery of safe and effective vaccines. Olfactory impairment is observed in over half of individuals with COVID-19, and ENT symptoms are widespread. While the vast majority of these patients experience spontaneous recovery, about 12% of them still experience OD persistence. This is a component of the Long COVID, another significant worldwide challenge. Hence, the management of persistent ENT symptoms by primary care and in the community, with appropriate referral to secondary care, needs to be mapped out. This must be accomplished in a comprehensive, person-centred manner that fits into the broader post-covid syndrome pathways. In addition, services should be delivered virtually wherever it is safe and appropriate.
LIST OF ABBREVIATIONS
| COVID-19 | = Coronavirus Disease 2019 |
| SARS-CoV-2 | = Severe Acute Respiratory Syndrome Coronavirus -2 |
| OD | = Olfactory Dysfunction |
| OT | = Olfactory Training |
CONSENT FOR PUBLICATION
Not applicable.
FUNDING
None.
CONFLICT OF INTEREST
The author declares no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


