All published articles of this journal are available on ScienceDirect.
Comparison, by Country, of the Uptake of COVID-19 Vaccination by Health Care Workers in the EU/EEA, January – June 2021
Abstract
Aims:
The aim of this study was to compare, by country, COVID-19 vaccination uptake by Health Care Workers (HCWs) from January to June 2021, to assist with policy making and prospective planning in these countries during the COVID-19 pandemic and into the future.
Background:
Health Care Workers (HCWs) are at high risk of exposure to COVID-19 when providing care to patients. We investigated the uptake of COVID-19 vaccination among HCWs in the EU/EEA and discussed the factors which influence this uptake.
Methods:
The study population included all the countries in the European Union (EU) and European Economic Area (EEA). The secondary data file was downloaded from the European Centre for Disease Prevention and Control (ECDC) website. Descriptive and comparative data were analysed and presented using Excel and Chi-square test of hypothesis.
Results:
The proportion of HCWs in EU/EEA countries ranged from 1.2% to 5.1% per population. From January to June 2021, the proportion of first and second dose vaccinations of HCWs ranged from 20% to 100% and from 21% to 100%, respectively. The Comirnaty–Pfizer/BioNTech vaccine (COM) was the most administered vaccine in all EU/EEA countries, followed by the Moderna mRNA-1273 vaccine (MOD) and the Astra-Zeneca–Vaxzevria vaccine (AZ). In January 2021, a median of 29% of HCWs received their first dose of COVID-19 vaccination. Italy was the only country with a mandatory vaccination policy for HCWs. Vaccination uptake rates were statistically different among EU countries (p<0.05).
Conclusion:
Data such as these could be used in mathematical modelling potential future pandemics to predict vaccine up-take by selected, exposed, vulnerable sectors of the population, for whom it is relevant.
1. INTRODUCTION
In December 2019, a pneumonia caused by a novel coronavirus (SARS-CoV-2) emerged. It was epi-centred in Hubei Province of the People’s Republic of China and rapidly spread around the world [1]. On 30th of January 2020, the WHO Emergency Committee declared a global health emergency based on growing case notification rates at Chinese and international locations [2]. Since December 2019, over 1.9 million SARS-CoV-2 confirmed fatalities have been recorded in the countries of the WHO European Region, with 90% in those aged 60 years and over [3]. Vaccines for SARS-CoV-2 save lives [4-6]. The clinical spectrum of COVID-19 varies from relatively asymptomatic to symptomatic forms, with the first symptoms usually appearing after five to six days [7]. Common symptoms include fever, fatigue, dry cough, sore throat, dyspnea, conjunctivitis and loss of taste and smell [8].
Health Care Workers (HCWs) are at high risk of exposure to COVID-19, both in the community and in the workplace when providing care to patients [9]. The median cumulative vaccine uptake among HCWs in the EU/EEA is over 90% for primary course vaccination with 51% receiving a booster dose [10]. This is however not uniform across Europe. We investigate the uptake of vaccination among HCWs in the EU/EEA and the factors which influence this uptake [11].
The aim of this paper is to compare, by country, COVID 19 vaccination uptake by HCWs from January to June 2021 and to assess any difference in vaccination uptake between these countries. This assists with policy making and prospective planning in these countries during the current pandemic and into the future. Vaccine development and the costs and contracts European countries have with manufacturers are discussed. Country specific policies relating to vaccination and mandatory vaccination are explored. The impact of HCW vaccination on the pandemic and the mortality of HCWs from COVID-19 is reviewed. The uptake of COVID-19 vaccination and vaccine hesitancy among HCWs is a significant issue and has been largely overlooked in evolving literature. This paper discusses vaccine hesitancy in this important group.
2. MATERIALS AND METHODS
Data collected by the ECDC and publicly available on the ECDC site were analysed [12, 13]. The data were presented in the Vaccine Tracker and collected through The European Surveillance System (TESSy). EU/EEA Member States were requested to report basic indicators and data by target groups at the national level once every two weeks.
The basic indicators included were the number of vaccine doses distributed by manufacturers, the number of first, second and additional doses given, and the number of doses refused. The type of vaccine given was also recorded. The population of each country and number of HCWs was documented. Target groups were categorised by age, HCWs and long-term care facility (LTCF) residents. Health care workers were defined as those who work in healthcare settings who may come into contact with patients, including clinical administration staff, and home care staff.
The data file was downloaded to Excel. There were 291,853 entries. Entries were made by all 30 countries of the EEA. The data file was condensed to include the target group of HCWs only. The member states were asked to record data every two weeks. The number of inputs over the study period, however, varied between 12 and 1789 per country. The data file was colour coded according to vaccine type. Excel equations were used to obtain the descriptive data seen in the results (Tables 1-7).
| Country | HCWn | HCW% of Population |
|---|---|---|
| Belgium (BE) | 522,242 | 4.5 |
| Bulgaria (BG) | 243,600 | 3.5 |
| Cyprus (CZ) | 354,319 | 3.3 |
| Denmark (DK) | 299,619 | 5.1 |
| Estonia (EE) | 16,472 | 1.2 |
| Greece (EL) | 274,955 | 2.6 |
| Spain (ES) | 2,180,000 | 4.6 |
| Croatia (HR) | 75,580 | 1.9 |
| Hungry (HU) | 172,621 | 1.8 |
| Ireland (IE) | 250,000 | 5.0 |
| Luxembourg (LU) | 16,477 | 2.6 |
| Latvia (LV) | 35,684 | 1.9 |
| Malta (MT) | 12,400 | 2.4 |
| Romania (RO) | 364,023 | 1.9 |
| Sweden (SE) | 123,200 | 1.2 |
| Slovenia (SI) | 43,611 | 2.1 |
Descriptive data were analysed using Excel and IBM SPSS Statistics version 27. Comparative data were analysed by Chi-square test of hypothesis.
3. RESULTS
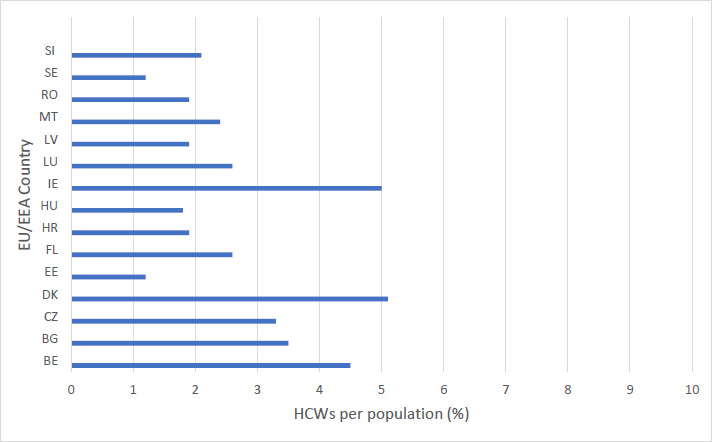
Of the thirty countries in the EU/EEA, twenty-one countries had inputs relating to HCWs and there were a total of 138,451 entries. The percentage of HCWs in EU/EEA countries, is illustrated below. It ranged from 1.2 to 5.1% per population. Estonia and Sweden had the lowest proportion of HCWs per population at 1.2%. Ireland and Denmark had the highest. Five percent of the Irish population were HCWs and 5.1% of the Danish population. The median value was 2.3%.
From January to June 2021, the percentage range of first dose vaccinations of HCWs ranged from 20% to 100%. Bulgaria had the lowest vaccination rate at 20%. Ireland and Hungary both achieved 100% vaccination of HCWs. The median value was 83% across all EU/EEA countries. From January to June 2021, 100% of HCWs in Ireland, Italy and Hungary received their second dose of the vaccine and were considered fully vaccinated. Bulgaria had the lowest value, with 21% receiving their second dose. The median was 80%.
The population denominators for HCWs were provided by reporting countries along with the vaccination data. As per the ECDC, the denominator data for HCWs reflected the official estimated number of HCWs in the country and may underestimate the total number of people enrolled as a HCW in the COVID-19 vaccination campaign. In these cases (Figs. 1-7) uptake figures in the vaccine tracker are capped at 100% [13]. Ireland, for example, had a first dose percentage of 126% and a second dose percentage of 122%. Hungary had a first dose percentage of 123% and a second dose percentage 115%. Italy administered 3,169,051 vaccines within the six-month period. Information, however, was not recorded on which a first or second dose or the number of HCWs in the country. This was 5.3% of the total population of Italy.
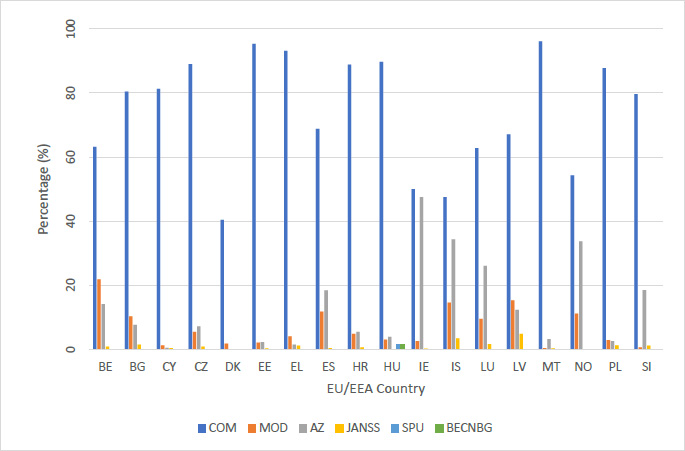
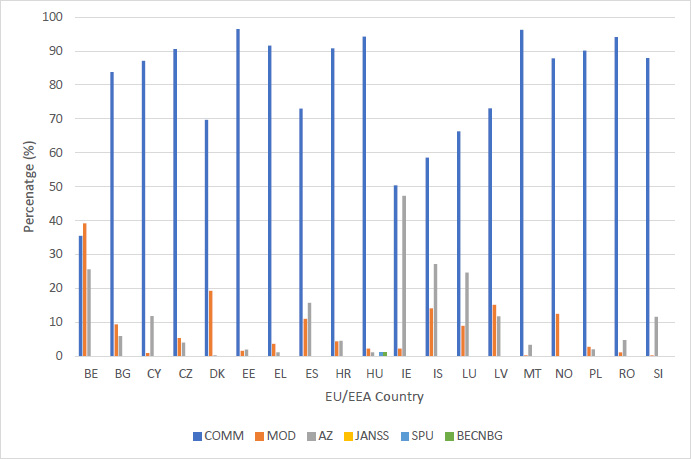
The Comirnaty – Pfizer/BioNTech vaccine (COM) was the most administered vaccine in every country except for Belgium. It had a first dose range of 40% to 100%. Denmark and Iceland had the lowest use of the Comirnaty vaccine during the first dose of vaccinations at 40% and 48%. Romania and Malta had the highest use at 100% and 96%, respectively. The median value was 80%. The use of the Comirnaty vaccine during the second dose vaccinations ranged from 36% to 96%. Belgium had the lowest use at 36% and Estonia had the highest at 96%. The median for the second dose was 87%.
The Moderna mRNA-1273 vaccine (MOD) was the second most used vaccine. Its use ranged from 0% to 22% for first dose and 0% to 39% for second dose. Moderna vaccine use was highest in Belgium, with 22% and 39% used during the first and second vaccination, respectively. Its use was low in Malta, Slovenia and Romania ranging from 0.3% to 1.2% during the first and second vaccination. The median value for Moderna was 4.1% and 4.2% for first and second dose, respectively. The AstraZeneca – Vaxzevria vaccine (AZ) use ranged from 0% to 35% for first dose and 0% to 47% for second dose. Its use was highest in Ireland and Iceland, with a first dose use of 47.5% and 34.4%, respectively. Its use was particularly low in Denmark at 0% and 0.3% for first and second dose.
The Janssen – Ad26.COV 2.5 vaccine (Janss) use ranged from 0.1% to 4.8% for the one dose vaccine. Latvia’s use of the vaccine was highest at 4.8%. Its use in all other countries ranged from 0% to 3.5%. Hungary was the only country that administered the Sputnik V vaccine (SPU). They administered 3,647 (2%) as a first dose and 2,160 (1%) as a second dose. Hungary was also the only country to administer the Beijing CNBG vaccine (BECNBG) and administered 3,251 (2%) as a first dose and 2,443 (1%) as a second dose.
| Country | 1st Dosen | % | 2nd Dosen | % | Valid Denominator |
|---|---|---|---|---|---|
| Belgium (BE) | 411,134 | 78.7 | 510,012 | 97.7 | 522,242 |
| Bulgaria (BG) | 49,202 | 20.2 | 50,520 | 20.7 | 243,600 |
| Cyprus (CY) | 2,922 | - | 3,468 | - | - |
| Czechia (CZ) | 308,010 | 86.9 | 286,921 | 80.4 | 354,319 |
| Denmark (DK) | 266,665 | 89.0 | 287,219 | 95.9 | 299,619 |
| Estonia (EE) | 13,697 | 83.1 | 12,647 | 76.8 | 16,472 |
| Greece (EL) | 206,068 | 74.9 | 197,471 | 71.8 | 274,955 |
| Spain (ES) | 2,008,861 | 92.1 | 1,867,191 | 85.7 | 2,180,000 |
| Croatia (HR) | 43,362 | 57.4 | 42,572 | 56.3 | 75,580 |
| Hungry (HU) | 212,559 | 100.0* | 198,914 | 100.0* | 172,621 |
| Ireland (IE) | 313,951 | 100.0* | 305,067 | 100.0* | 250,000 |
| Iceland (IS) | 25,409 | - | 25,764 | - | - |
| Italy (IT) | - | - | - | 100.0* | - |
| Luxembourg (LU) | 12,040 | 73.1 | 11,945 | 72.5 | 16,477 |
| Latvia (LV) | 19,991 | 56.0 | 20,139 | 56.4 | 35,684 |
| Malta (MT) | 12,107 | 97.7 | 12,014 | 96.8 | 12,400 |
| Norway (NO) | 270,155 | - | 208,396 | - | - |
| Poland (PL) | 988,694 | - | 1,012,640 | - | - |
| Romania (RO) | 302,032 | 83.0 | 318,689 | 87.5 | 364,023 |
| Sweden (SE) | 103,400 | 83.9 | 76,800 | 62.3 | 123,200 |
| Slovenia (SI) | 28,129 | 64.5 | 28,437 | 65.2 | 43,611 |
| - | COM | MOD | AZ | JANSS | Denominator* |
|---|---|---|---|---|---|
| 1st Dose2nd Dose | 1st Dose2nd Dose | 1st Dose2nd Dose | One Dose | 1st Dose2nd Dose | |
| n (%) | n (%) | n (%) | n (%) | - | |
| Belgium (BE) | 259,718(63.2)180,884(35.5) | 89,572(21.8) 199,688(39.2) | 57,907(14.1) 130,431(25.6) | 3,532(0.9) | 411,134510,012 |
| Bulgaria (BG) | 39,539(80.4) 42,318(83.8) | 5,051(10.3) 4,793(9.5) | 3,788(7.7) 3,017(6.0) | 735(1.5) | 49,20250,520 |
| Cyprus (CY) | 2,375(81.3) 3,021(87.1) | 38(1.3) 35(1.0) | 14(0.5) 412(11.9) | 11(0.4) | 2,9223,468 |
| Czechia (CZ) | 273,916(89.0) 259,575(90.5) | 16,775(5.5) 15,446(5.4) | 22,168(7.2) 11,900(4.1) | 2,760(0.9) | 308,010286,921 |
| Denmark (DK) | 107,787(40.4) 200,133(69.7) | 4,822(1.8) 55,333(19.3) | 13(0.0) 798(0.3) | 22(0.0) | 266,665287,219 |
| Estonia (EE) | 13,048(95.3) 12,199(96.4) | 290(2.1) 201(1.6) | 320(2.3) 247(2.0) | 39(0.3) | 13,69712,647 |
| Greece (EL) | 192,018(93.2) 180,794(91.6) | 8,450(4.1) 7,244(3.7) | 3,100(1.5) 2,274(1.2) | 2,500(1.2) | 206,068197,471 |
| Spain (ES) | 1,381,795(68.8) 1,363,786(73.0) | 237,051(11.8) 204,037(11.0) | 370,288(18.4) 294,780(15.8) | 8,500(0.4) | 2,008,8611,867,191 |
| Croatia (HR) | 38,557(88.9) 38,657(90.8) | 2,120(4.9) 1,894(4.4) | 2,401(5.5) 1,964(4.6) | 257(0.6) | 43,36242,572 |
| Hungry (HU) | 190,602(89.7) 187,304(94.2) | 6,560(3.1) 4,634(2.3) | 8,250(3.9) 2,373(1.2) | 249(0.1) | 212,559198,914 |
| Ireland (IE) | 155,975(50.0)153,825(50.4) | 8,199(2.6)6,909(2.3) | 149,216(47.5)144,333(47.3) | 561(0.2) | 313,951305,067 |
| Iceland (IS) | 12,063(47.5)15,095(58.6) | 3,710(14.6)3,664(14.2) | 8,753(34.4)7,002(27.2) | 883(3.5) | 25,40925,764 |
| Luxembourg (LU) | 7,568(62.8)7,916(66.3) | 1,138(9.5)1,076(9.0) | 3,140(26.1)2,953(24.7) | 194(1.6) | 12,04011,945 |
| Latvia (LV) | 13,413(67.1)14,718(73.1) | 3,068(15.3)3,060(15.2) | 2,459(12.3)2,361(11.8) | 956(4.8) | 19,99120,139 |
| Malta (MT) | 11,635(96.1)11,565(96.2) | 48(0.4)34(0.3) | 391(3.2)414(3.4) | 33(0.3) | 12,10712,014 |
| Norway (NO) | 146,866(54.3)182,172(87.4) | 30,351(11.2)26,033(12.5) | 91,002(33.7)190(0.1) | 30(0.0) | 270,155208,396 |
| Poland (PL) | 868,412(87.8)912,599(90.1) | 29,062(2.9)28,306(2.8) | 75,873(2.6)21,341(2.1) | 12,382(1.3) | 988,6941,012,640 |
| Romania (RO) | 312,154(100.0)299,774(94.1) | 1,768(0.6)3,708(1.2) | 17,565(5.8)15,207(4.8) | 1,342(0.4) | 302,032318,689 |
| Slovenia (SI) | 22,414(79.7)25,000(87.9) | 184(0.6)92(0.3) | 5,193(18.5)3,305(11.6) | 338(1.2) | 28,12928,437 |
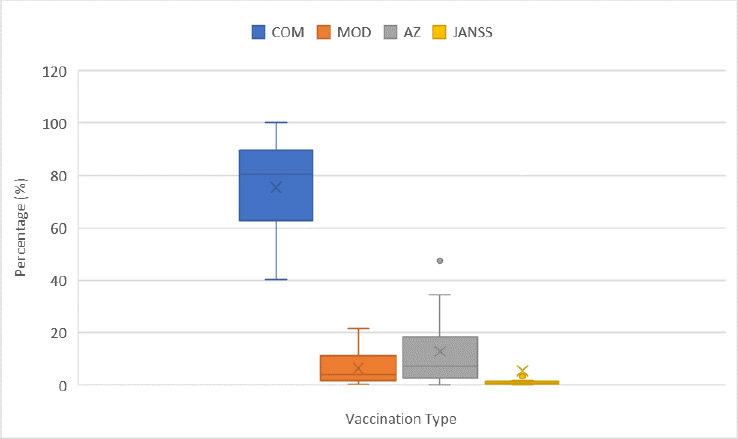
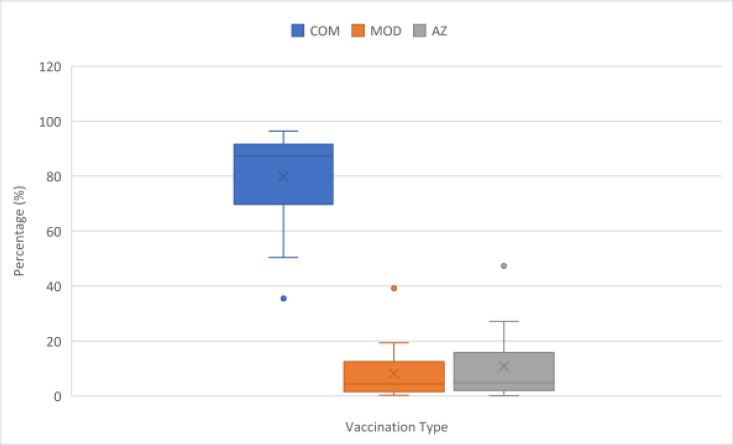
| Vaccination | - | 1st Dose(%) | 2nd Dose(%) |
|---|---|---|---|
| COM | Median | 80.8 | 87.4 |
| Range | 40.4-100.0 | 35.5-96.7 | |
| |25-75| | 62.7-91.4 | 71.4-92.9 | |
| MOD | Median | 4.1 | 4.9 |
| Range | 0.4-21.8 | 0.3-39.2 | |
| |25-75| | 2.0-11.5 | 1.6-12.5 | |
| AZ | Median | 7.5 | 4.8 |
| Range | 0.5-47.5 | 0.1-47.3 | |
| |25-75| | 3.2-18.5 | 2.0-15.8 | |
| Janss | Median | 0.9 | - |
| Range | 0.1-4.8 | - | |
| |25-75| | 0.4-1.4 | - |
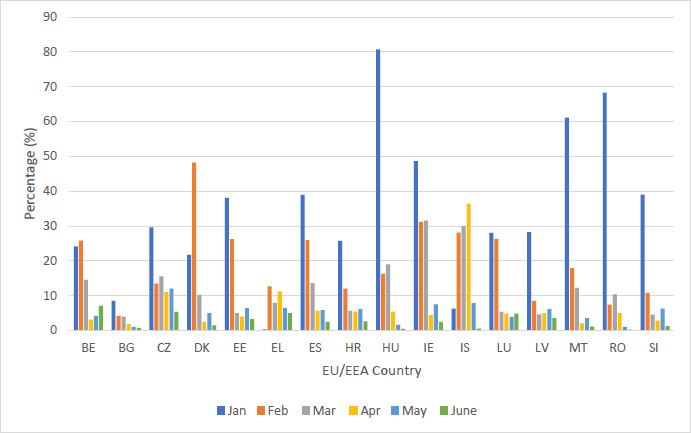
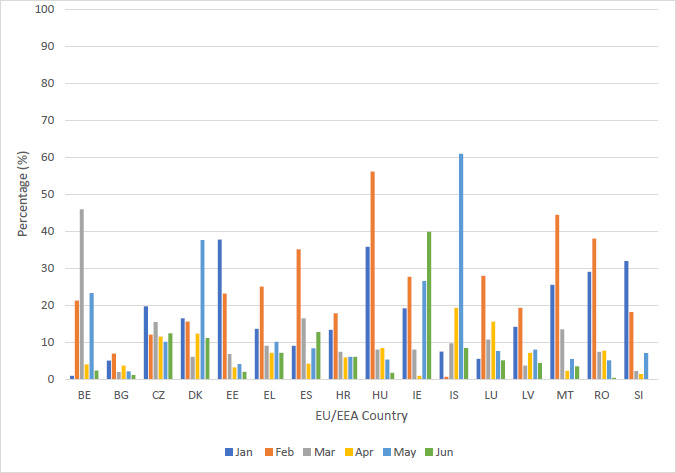
| Country | Jan | Feb | Mar | Apr | May | Jun | - |
|---|---|---|---|---|---|---|---|
| 1st dose2nd dose | 1st dose2nd dose | 1st dose2nd dose | 1st dose2nd dose | 1st dose2nd dose | 1st dose2nd dose | Denominator* | |
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | ||
| Belgium (BE) | 126,070(24.1)4,616(0.9) | 134,919(25.8)110,802(21.2) | 75,807(14.5)239,631(45.9) | 16,071(3.1)20,990(4.0) | 21,848(4.2)121,849(23.3) | 36,419(7.0)12,121(2.3) | 522,242 |
| Bulgaria (BG) | 20,800(8.5)12,270(5.0) | 10,225(4.2)16,753(6.9) | 9,771(4.0)4,592(1.9) | 4,390(1.8)9,108(3.7) | 2,385(1.0)5,221(2.1) | 1,631(0.7)2,576(1.1) | 243,600 |
| Cyprus (CY) | 1,8861,480 | 5631,384 | 31070 | 7093 | 84356 | 985 | - |
| Czechia (CZ) | 104,779(29.6)69,672(19.7) | 47,461(13.4)42,281(12.0) | 54,979(15.5)54,554(15.4) | 39,224(11.0)40,674(11.5) | 42,627(12.0)35,690(10.1) | 18,940(5.3)44,050(12.4) | 354,319 |
| Denmark (DK) | 65,023(21.7)49,248(16.4) | 144,424(48.2)46,890(15.6) | 30,570(10.2)18,064(6.0) | 7,334(2.4)26,819(12.3) | 15,016(5.0)112,794(37.6) | 4,298(1.4)33,404(11.1) | 299,619 |
| Estonia (EE) | 6,280(38.1)6,209(37.7) | 4,330(26.2)3,798(23.1) | 829(5.0)1,117(6.8) | 672(4.0)534(3.2) | 1,059(6.4)670(4.1) | 527(3.2)319(2.0) | 16472 |
| Greece (EL) | 87,237(0.3)37,407(13.6) | 34,573(12.6)68,600(25.0) | 21,626(7.9)24,689(9.0) | 30,850(11.2)19,607(7.1) | 17,942(6.5)27,738(10.1) | 13,840(5.0)19,429(7.1) | 274,955 |
| Spain (ES) | 848,255(38.9)195,081(9.0) | 563,910(25.9)765,727(35.1) | 295,685(13.6)357,417(16.4) | 122,000(5.6)91,516(4.2) | 125,739(5.8)180,697(8.3) | 53,272(2.4)276,753(12.7) | 2,180,000 |
| Croatia (HR) | 19,413(25.7)10,076(13.3) | 9,009(12.0)13,477(17.8) | 4,252(5.6)5,565(7.4) | 4,079(5.4)4,458(5.9) | 4,633(6.1)4,526(6.0) | 1,976(2.6)4,470(6.0) | 75,580 |
| Hungry (HU) | 139,368(80.7)61,815(35.8) | 27,951(16.2)96,861(56.1) | 32,680(19.0)13,741(8.0) | 9,239(5.4)14,429(8.4) | 2,712(1.6)9,170(5.3) | 609(0.4)2,898(1.7) | 172,621 |
| Ireland (IE) | 121,387(48.6)47,736(19.1) | 77,919(31.2)69,318(27.7) | 78,786(31.5)20,023(8.0) | 11,119(4.4)2,359(0.9) | 18,810(7.5)66,161(26.5) | 5,930(2.4)99,473(39.8) | 250,000 |
| Iceland (IS) | 1,450(6.3)1,702(7.5) | 6,410(28.1)1,601(0.6) | 6,861(30.0)2,218(9.7) | 8,310(36.4)4,409(19.3) | 1,772(7.8)13,921(60.9) | 106(0.5)1,913(8.4) | 22,845 |
| Luxembourg (LU) | 4,606(28.0)911(5.5) | 4,341(26.3)4,605(27.9) | 870(5.3)1,761(10.7) | 794(4.8)2,574(15.6) | 639(3.9)1,250(7.6) | 790(4.8)844(5.1) | 16,477 |
| Latvia (LV) | 10,073(28.2)5,041(14.1) | 3,052(8.5)6,896(19.3) | 1,655(4.6)1,309(3.7) | 1,781(4.9)2,524(7.1) | 2,169(6.1)2,837(8.0) | 1,261(3.5)1,532(4.3) | 35,684 |
| Malta (MT) | 7,571(61.1)3,167(25.5) | 2,218(17.9)5,501(44.4) | 1,513(12.2)1,971(13.5) | 242(2.0)273(2.2) | 431(3.5)669(5.4) | 132(1.1)433(3.5) | 12,400 |
| Norway (NO) | 33,6161,258 | 84,39937,770 | 52,3237,299 | 36,7636,425 | 13,178122,284 | 49,87633,360 | - |
| Poland (PL) | 611,927251,830 | 83,255454,680 | 109,82655,542 | 101,22849,663 | 4,1862119,209 | 40,59681,716 | - |
| Romania (RO) | 248,658(68.3)105,249(29.0) | 26,865(7.4)138,356(38.0) | 37,237(10.3)27,030(7.4) | 18,139(5.0)27,925(7.7) | 3,699(1.0)18,464(5.1) | 738(0.2)1,483(0.4) | 364,023 |
| Slovenia (SI) | 17,008(39.0)13,924(31.9) | 4,689(10.8)7,890(18.1) | 1,957(4.5)942(2.2) | 1,219(2.8)616(1.4) | 2,745(6.3)3,069(7.0) | 511(1.2)1,996(4.6) | 43,611 |
In January 2021, a median of 29% of HCWs received their first dose of COVID-19 vaccination. Fifteen percent received their second dose of vaccine. In February 2021, 17% received their first and 22% received their second COVID-19 vaccination. In March 2021, 10% of HCWs received their first dose of vaccination and 8% received their second. In April, May and June 5, 6% and 2% of HCWs received the first vaccine and 7%, 8%, and 5% received a second dose of the vaccine.
| Vaccination | - | 1st Dose(%) | 2nd Dose(%) |
|---|---|---|---|
| Jan | Median | 28.9 | 15.3 |
| Range | 0.3-80.7 | 0.9-37.7 | |
| |25-75| | 23.0-43.8 | 8.3-27.3 | |
| Feb | Median | 16.2 | 23.1 |
| Range | 4.2-48.2 | 0.6-56.1 | |
| |25-75| | 10.8-26.2 | 17.8-27.9 | |
| March | Median | 11.2 | 8.0 |
| Range | 4.0-31.5 | 1.9-45.9 | |
| |25-75| | 5.2-15.9 | 6.4-12.1 | |
| Apr | Median | 4.9 | 6.5 |
| Range | 1.8-36.4 | 0.9-19.3 | |
| |25-75| | 3.0-5.5 | 3.2-10.0 | |
| May | Median | 6.0 | 7.8 |
| Range | 1.0-12.0 | 2.1-60.9 | |
| |25-75| | 3.7-6.5 | 5.4-16.7 | |
| June | Median | 2.4 | 4.9 |
| Range | 0.2-7.0 | 0.4-39.8 | |
| |25-75| | 0.9-4.2 | 2.2-9.8 |
| Country | HCWPercentage (%) | FullyVaccinatedHCWs (%) | TotalPopulation | Totaldoses given | HCWNumber | Significance |
|---|---|---|---|---|---|---|
| Italy | 1.3 | 100* | 59,641,488 | 3,169,051 | 753,836b | P<0.05a |
| Spain | 4.6 | 85.7 | 47,332,614 | 3,876,052 | 2,180,000 | - |
| Slovenia | 2.1 | 65.2 | 2,095,861 | 180,200 | 43,611 | - |
| Belgium | 4.5 | 97.7 | 11,522,440 | 921,146 | 522,242 | - |
| Greece | 2.6 | 71.1 | 10,718,565 | 403,539 | 274,955 | - |
During the period of January to June 2021, Italy was the only country in the EU/EEA to have a mandatory vaccination policy in place for HCWs. Vaccination uptake in Italy was compared with four other EU countries. These EU countries were chosen based on their similar demographics, culture, governments, infrastructure and geography. These countries have a predominantly Catholic religion and democratic governments. They have a similar economy and currency. They have similar climates, infrastructure and geography with most being mountainous and bordering the Mediterranean sea. HCWs who received two doses of vaccination were considered fully vaccinated. Italy, however, did not report their total HCW number with the vaccination data to the ECDC. A HCW percentage of 1.3% was used, as per the Italian National Statistics Office, during the study period of January to June 2021 [14, 15]. There was a statistically significant difference in vaccination rates between the five EU countries.
4. DISCUSSION
Health care workers are at high risk of exposure to COVID-19 in the workplace when providing care to patients [9]. The median cumulative vaccine uptake among HCWs in the EU/EEA is currently over 90% for primary course vaccination with 51% receiving a booster dose [10]. This is, however, not uniform across Europe. We investigate the uptake of vaccination among HCWs in the EU/EEA over a six-month period and the factors which influence this uptake [11].
A study by the WHO Regional Office for Europe and ECDC published in Eurosurveillance in November 2021, estimates that 470,000 lives have been saved among those aged 60 years and over since the start of COVID-19 vaccination roll-out in 33 countries across the WHO European Region. This estimate does not include lives saved by vaccination in those under 60 years old or lives saved from the indirect effect of vaccination because on transmission Harvard referencing - please replace with vancouver [11].
At the time of this study, Italy was the only European country that had mandatory vaccination for HCWs. Mandated medical intervention, such as vaccination, is a contentious issue. Health care professionals have personal rights but also special obligations. Professionals who care for patients accept an overriding ethical imperative embodied in the Hippocratic Oath [14]. Unvaccinated workers who could potentially spread COVID-19 can cause huge harm. This is especially true with vulnerable patients such as those in intensive care units or on chemotherapy treatment. Patients have the right to expect their hospital will take every reasonable precaution to protect them from contracting a new disease upon admission to hospital. Vaccination is one of the main ways to avoid this. Voluntary compliance by health care professionals is preferable, however, to mandates [15].
Vaccine hesitancy is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience and confidence [16]. Studies have shown a varying but often substantial proportion of HCWs are hesitant about receiving COVID-19 vaccinations. Health professionals often do not voice their concerns, particularly to colleagues, due to the institutional and societal pressures to vaccinate [17]. A scoping review of HCWs’ hesitancy to be COVID-19 vaccinated found that 23% out of 76,417 HCWs worldwide were hesitant about the available vaccines. Their main concerns (safety, efficacy, and side effects) were very similar to the concerns identified by the general public [18].
Health care workers suggested four major areas of focus to improve vaccination compliance. These included improved information, involvement of health authorities or other regulators, ensuring skilled communication between HCWs and patients, and improved training of HCWs [12]. It is vital that strategies to improve vaccination uptake focus on these concerns and are adapted to the specific political, social, cultural and economic context of the country in question. Improving vaccine confidence among HCWs is crucial, as it has been shown to influence patient vaccination uptake [10].
Reliance on social media, newspaper and television for vaccine information was shown to have a negative impact on vaccination uptake. A substantial relationship between disinformation campaigns and declining vaccination coverage was also shown [19, 20]. Barriers to COVID-19 vaccination among ethnic minority groups included pre-existing mistrust of formal services, lack of information about the vaccine’s safety, misinformation, inaccessible communications, and logistical issues [21].
This paper provides descriptive and analytical analysis of a very large dataset from EU/EEA countries. It provides vaccination uptakes numbers and percentages for HCWs across EU/EEA countries for research and modelling purposes. Healthcare workers were defined as those who work in healthcare settings who may come into contact with patients, including clinical admin-istration staff, and home care staff. This was determined by the reporting country. The dataset was incomplete. There was inconsistency in reporting rates which varied across the countries. There were gaps in reporting. This leads to a questionable internal validity due to both variable intra-rater and inter-rater reliability rates. The data related to EU/EEA countries and therefore lack generalisability to non-EU/EEA countries. Countries were asked to report uptake numbers twice weekly. Most countries, however, had many more inputs than two per week. Therefore, they may be some recall or response bias. This is important to address for ongoing data collection. The importance of complete reporting should be emphasised to facilitate reliable research.
COVID-19 vaccine supply was an important limiting factor affecting uptake in these EU/EEA countries. Other factors, however, such as vaccine hesitancy among HCWs need to be considered [12]. Vaccination uptake among HCWs was poor in several countries despite supply [11,13]. To aid future planning and policy development, including mandatory vaccination policies, analysis of large secondary datasets such as these is crucial. Analysis allows for descriptive and comparative data ultimately to aid emergency planning and vaccination modelling for the future [22]. If leveraged appropriately, analysis such as this can assist policy makers and public health officials to understand vaccine uptake rates and craft policies to improve them [23, 24].
Public Health authorities, governments and HCWs have a duty to highlight threats to public health. Effective public relations and communication should be utilised to elicit an appropriate and measured response from the population. Sandman (1993) describes how an appropriate public response to a particular threat can be achieved. In public policy and disease management, the outrage factor is public opposition to a policy, such as mandatory vaccination, or public fear relating to a particular disease that is not based on the knowledge of the technical details. It is a combination of the threat and the outrage of the population. The importance of responding to community outrage and strategies for effective risk communication should be employed to elicit an appropriate public response to COVID-19 and other further diseases [25].
The degree of public awareness of the condition and the perceived severity of the condition should be considered. Several models of health promotion, including the Health Belief Model can be utilised to assess whether a person will take a health-related action. Individuals will adopt health-related actions if they believe that they are faced with risk and have the potential to reduce that risk. If a person believes that they are susceptible to a condition, that the condition could potentially have serious consequences and that there is a course of action available to reduce this risk, then they are more likely to adopt this course of action. The person must believe that the benefit of the action outweighs the costs or barriers and that they have the ability to carry out the action [26]. Health promotion strategies and policies should focus on these factors to reduce vaccination hesitancy and increase vaccination uptake in HCWs and the population in general. Effect, accessible and reliable provision of information by Public Health in essential to achieving this [26].
Vaccination is cost effective. It reduces infection rates, hospitalisations and deaths [28]. Cheong et al. (2021) described how despite the widespread accessibility of COVID-19 vaccines across the US, vaccination rates have become stagnant, necessitating predictive modelling to identify important factors impacting vaccination uptake [24]. Other studies have examined the effects of low vaccine uptake, due to vaccine hesitancy, for the current COVID-19 pandemic and have shown the impact of vaccine hesitancy on mortality [29]. Results also further support the idea of the indirect benefits of vaccination, which are necessary to achieve herd immunity [29].
Alvarez et al. (2021) developed a demographic mathematical model that considers social distancing, intensity of the testing effort, vaccination coverage, and vaccination rate to predict the evolution of pandemic COVID-19 in urban areas. Results suggest that the rate of vaccination is more important than the overall vaccination coverage for containing COVID-19. In addition, the modelling indicates that widespread testing and quarantining of infected subjects greatly benefit the success of vaccination campaigns [30].
CONCLUSION
Analysis such as this could be used in a prospective way. Through mathematical modelling, for example, it could be used in future potential pandemics in order to predict vaccine uptake by selected, exposed, vulnerable sectors of the population, for whom it is relevant. Country specific models could be developed with variables such as vaccine supply, HCW vaccination rates, mandatory vaccination status, vaccination type and hesitancy rates. These simple models could be used as a friendly, readily accessible, and cost-effective tool for assisting health officials and local governments in the rational design and planning of vaccination strategies.
LIST OF ABBREVIATIONS
| HCWs | = Health Care Workers |
| EU | = European Union |
| EEA | = European Economic Area |
| ECDC | = Disease Prevention and Control |
| MOD | = Moderna mRNA-1273 vaccine |
| AZ | = Astra-Zeneca–Vaxzevria vaccine |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Not applicable.
HUMAN AND ANIMAL RIGHTS
No animals/humans were used in this research.
CONSENT FOR PUBLICATION
Not applicable.
AVAILABILITY OF DATA AND MATERIALS
The data and supportive information is are available within the article.
FUNDING
None.
CONFLICT OF INTEREST
The authors declare no conflict of interest financial or otherwise.
ACKNOWLEDGEMENTS
Declared none.


