All published articles of this journal are available on ScienceDirect.
COVID-19 Vaccination Acceptance and its Predicting Factors among Internet Users in Ho Chi Minh City and Other Regions in Vietnam
Abstract
Aim:
This study was conducted to evaluate the acceptance of COVID-19 vaccination and its predictors among adult internet users residing in Ho Chi Minh City (HCMC) and other regions in Vietnam.
Methods:
An online survey was disseminated to eligible participants, applying the snowball sampling technique, including demographic details, knowledge, five components of the Health Belief Model (HBM), and acceptance of COVID-19 vaccination. Logistic regression analysis was employed to determine predicting factors toward COVID-19 vaccination acceptance.
Results:
Among 3310 participants, the majority were 18-39 years old (76.1%), and had completed higher education (69.7%). Most respondents reported sufficient knowledge (90.2%). 87.8% showed acceptance of getting COVID-19 vaccinated. While becoming unemployed (OR = 0.70, 95% CI 0.52-0.94), the number of chronic diseases (OR = 0.76, 95% CI 0.65-0.89), living in the environment with currently existing infected cases (OR = 0.68, 95% CI 0.50-0.93), and perceived barriers (OR = 0.88, 95% CI 0.85-0.91) were negative determinants, the number of information sources for updating COVID-19 vaccine (OR = 1.10, 95% CI 1.01-1.19), perceived benefits (OR = 1.12, 95% CI 1.07-1.18), and cues to action (OR = 1.23, 95% CI 1.18-1.29) were positive predictors for vaccination acceptance.
Conclusion:
The internet users’ level of acceptance of COVID-19 vaccination was impressively high and influenced by perceived benefits, barriers, cues to action, and some demographic and health-related details. People with low acceptance levels, such as chronically ill adults, should be imported into consideration and provided with reliable scientific information.
1. INTRODUCTION
Since its first detection in December 2019 in Wuhan, China, the coronavirus disease 2019 (COVID-19) has been increasingly threatening as a global health challenge with several waves of torrential attacks [1, 2]. To straighten this curve and end the pandemic, organizations, governments, and countries have made a series of great efforts on a global scale [2]. Despite these efforts, the world is still facing an unprecedented health crisis, with 222 countries invaded by the coronavirus, nearly 190 million infected cases, and more than 4 million deaths, making up the mortality rate at 2.16% [3]. On July 6th, 2021, Vietnam recorded 19,933 confirmed cases [4], signaling the rebounding of the virus in this country. In addition, several novel variants of the virus have also been detected in many countries, with faster speed and various modes of transmission. From these evidence, it is undeniable that current surface prevention strategies for COVID-19 seem somewhat ineffective. Therefore, developing strategies to generate community immunity from an individual level is important.
Herd immunization by vaccination against COVID-19 has been reported to be safe, effective, and attracting worldwide attention [5, 6]. A growing body of evidence has supported the protective efficacy of vaccination against COVID-19 [7-14] that vaccinated individuals are more likely to be protected from required hospitalization if infected, compared with non-immune individuals. Mortality from infection in the vaccinated population was also reported to be significantly lower than in the control group. Therefore, the earlier the establishment of individual and herd immunity by COVID-19 vaccination is completed, the higher the protective effects are achieved. The spreading of COVID-19 is believed to successfully end once a high herd immunity threshold at 55-85% has been reached [15] by decreasing the probability of susceptible individuals getting exposed to infectious sources.
However, although health agencies and governments have been making great efforts to raise COVID-19 herd immunity coverage, the proportion of people’s willingness to receive the COVID-19 vaccine varied widely across countries, ranging from very low (< 50%) [16-22], moderate (50-70%) [23-36] to significantly high (> 70%) [37-45].
In addition, the willingness for COVID-19 vaccination was also influenced by many factors. To be detailed, the probability of vaccination orientation was found to be positively related to perceptions of severity or vulnerability to COVID-19 [46, 47], awareness of the benefits of COVID-19 vaccination [20, 26, 46, 47], beliefs on vaccine safety [26, 35, 37, 48], sufficient knowledge regarding the disease [46], high education level [18, 29, 31, 47], history of vaccination in the past [37, 47, 49], elderly [43], undergoing chronic diseases [44, 49], getting married [37] and some others. Furthermore, other features, such as unemployment, low income or no insurance [23], non-medical occupational background [43] were reported to hinder people’s vaccination decisions. In addition, some factors have shown an inconsistent correlation in some studies, such as gender [19, 26, 44].
In Vietnam, little is known about the community’s willingness to receive COVID-19 vaccination and its predictors. A few studies were conducted previously on the intention to vaccinate against COVID-19 among healthcare workers, adult patients with chronic illness, and health science students, with the found proportions at 76.1% [46], 84.0% [50], and 77.7% [51] respectively. However, the surveys in these works were delivered to the target population when the COVID-19 pandemic status in Vietnam was still under well control [52], and the arrival of a potential COVID-19 vaccine shipment had yet to be confirmed. Furthermore, the acceptance of vaccination seemed to vary over time under different conditions, resulting in the unavailability of reliable data regarding the level of intention to get COVID-19 vaccination in the current pandemic outbreak status.
Community vaccination is an undelayable action to find a drastic solution to the threat of COVID-19 in the current context. Therefore, it is important to conduct a large-scale investigation into the knowledge, belief, and acceptance of the affected community for COVID-19 vaccination under the present circumstances. Updated and broadly representative evidence is essential to provide valuable data in the new situation, which is helpful to develop or change strategies and promote the speed and effectiveness of COVID-19 herd immunity. Therefore, this study was conducted to evaluate the acceptance to receive COVID-19 vaccination and its predictors among the Vietnamese people in the regions that were strongly affected by the current COVID-19 relapse, including Ho Chi Minh City and some other areas. To adapt to the lockdown condition during the pandemic, we decided to distribute the survey to participants via the internet.
2. METHODS
2.1. Design, Participants, and Recruitment
An anonymous online survey in this cross-sectional study was disseminated to those aged at least 18 years, fluent in Vietnamese, currently residing in Vietnam, and voluntarily participating in the work from July 26 to August 15, 2021, with the snowball sampling technique from the origin of researchers’ networks that was also utilized in other works to comply with the strict social distancing and restrictions on movement [20, 25, 36, 39, 53], using the most popular social network platforms in this country (Facebook, Zalo, Skype, Viber). To enhance the diversity of the study population characteristics, those who completed this questionnaire would be encouraged to forward the survey linkage to all contacts on their networks regardless of the provincial border.
2.2. Study Instrument
The 8-part questionnaire was developed through a comprehensive literature review, which investigated (A) demographic and health details and assessed (B) general knowledge of COVID-19. The next sections, closely following the Health Belief Model (HBM) that was widely adopted to predict a person's likelihood of performing a health action [54, 55], examined subjects’ perceptions related to COVID-19 and COVID-19 vaccination, including (C) perceived susceptibility and (D) perceived severity of COVID-19, (E) perceived benefits and (F) perceived barriers of COVID-19 vaccination, and (G) cues to action, measured with statements under the form of 5-point Likert scale, ranging from 1 (as totally disagree) to 5 (as totally agree). To improve the reliability of the scales, 2 reversed items were added in sections D and E to check the response orientation of study subjects. The mean scores of each subscale from C to G were calculated. For the knowledge element, one point would be assigned for each correct answer, yielding a total score of 5. By employing Bloom's cut-off classification, participants would be considered sufficiently knowledgeable if they answered correctly at least 80% of the questions in part B (equivalent to ≥ 4 points) [56-58].
The dependent variable in section H captured via a 5-point-scale statement, “As soon as I am on the vaccination list, I would agree to get COVID-19 vaccinated,” was classified into two categories: acceptance (definitely agree or agree) or reluctance (definitely disagree, disagree or uncertain). Participants were also asked on a 5-point scale if they would be willing to recommend their contacts to get the COVID-19 vaccine in the absence of any contraindications.
A panel of three experts in the fields of scientific research, clinical psychology, and public health ascertained the measurement clarity, validity, succinctness, reliability, and interestingness [59]. Then, 30 eligible participants were asked whether the revised questionnaire was understandable. The Cronbach Alpha values of elements C, D, E, F, and G were also calculated, revealing acceptable reliabilities of 0.74, 0.82, 0.73, 0.60, and 0.84, respectively.
2.3. Data Refinement
Prior to the analysis process, meticulous refinement and scrutiny were carried out to eliminate incomplete or dishonest responses caused by their nature as a self-completed online survey. Responses with the answering time recorded by the system longer than 30 minutes or questions in elements D and E had the same choice field (except for value “no opinion/unknown”) considered inactive or unintentional participation would also not be included in analysis.
2.4. Data Analysis
The tables with means, standard deviations, frequency, and proportion were used for data summarization. The χ2 test was performed to examine differences in vaccination acceptance rates as binary variables across demographic categories. Meanwhile, odds ratio (OR) and 95% confidence intervals (95% CI), followed by running multivariable logistic regression analysis, were adopted to determine predicting factors for COVID-19 vaccination willingness. The p-value indicating the statistically significant difference was set at under 0.05. Two pie charts were also drawn to visualize the distribution of vaccination acceptance by the subjects. All these statistics were generated on IBM SPSS Statistics for Windows, version 26.0 (IBM Corp., Armonk, NY, the USA).
2.5. Ethical Approval
In compliance with the Helsinki Declaration, this study had also been ethically approved by the Medical Ethics Committee of University Medical Center Ho Chi Minh City, Vietnam, before its data collection stage proceeded (Approval No.77/GCN-HĐĐĐ-UMC, 26/7/2021). The respondents were first required to show their consent by answering a required question in the introductory part of the survey if they were willing to go through the survey as a participant in the study. Confidentiality was guaranteed as researchers only accessed the data. Furthermore, following the ethics principle, no personal identifiers were collected in this study.
3. RESULTS
3.1. Socio-demographic Characteristics
Out of 3384 people reaching the questionnaire, 3310 fully responded, yielding a 97.8% completion rate (71 indicated their unwilling participation, and three were not eligible to participate since they were younger than 18). Table 1 provides a descriptive summarization of the data. Overall, the gender distribution of respondents was in favor of women (65.0%). While the mean age of subjects was 34.21 (SD=10.09, 18-81), the higher proportion of them was in the 18-39 group (76.1%) across the 18-81 age strata. Those graduating with a diploma, college, or university degree accounted for more than two-thirds (69.7%) of participants. 40.9% of this sample were healthcare workers or those working in medical areas. Half of the respondents shared their living space with subjects vulnerable to COVID-19 (children, the elderly older than 70, the pregnant, or people with underlying health conditions) (52.6%). Up to 2076 respondents rated their overall health as good or very good (62.7%), and roughly two-thirds were chronic disease-free (n = 2264). The participants were recorded with wide geographic distribution, but they were mainly from Ho Chi Minh City (81.5%) and urban areas (89.4%). Their overall economic capacity model had a skewed dispersion with approximately equal high rates of low-income and middle-income (39.5% and 39.8%, respectively), compared with the high-income category (20-30 or higher than 30 million Vietnam dong). However, less representation of ethnic minorities (4.0%) was observed in this study. Besides, almost all participants reported that they mostly heard about COVID-19 vaccination via social media on the internet (87.0%).
| Characteristics | n | % |
|---|---|---|
|
Age (years) (Mean ± SDa (min-max)) 18 – 39 40 – 59 ≥ 60 |
34.21±10.09 (18–81) | |
| 2519 712 79 |
76.1 21.5 2.4 |
|
|
Gender Male Female |
1160 2150 |
35.0 65.0 |
|
Education Level ≤ High school Vocational, school/college/University ≥ Post-graduate |
199 2307 804 |
6.0 69.7 24.3 |
|
Ethnicity Kinh Ethnic minorities |
3176 134 |
96.0 4.0 |
|
Religion/Religious Belief Buddhism Christian Others None |
542 378 36 2354 |
16.4 11.4 1.1 71.1 |
|
Marital Status Unmarried/widowed/divorced Married |
1470 1840 |
44.4 55.6 |
|
Geographic Zone Ho Chi Minh City Others |
2696 614 |
81.5 18.5 |
|
Region of Residence Urban Rural |
2960 350 |
89.4 10.6 |
|
Living Status Alone With vulnerable people With others |
353 1743 1214 |
10.7 52.6 36.7 |
|
Occupation Student Healthcare-related worker Professional/Technician Public servant/ Self-employed/Others Housewife/Retiree |
381 1355 844 631 99 |
11.5 40.9 25.5 19.1 3.0 |
|
Employment Status Unchanged From employed to unemployed From unemployed to employed |
2641 650 19 |
79.8 19.6 0.6 |
|
Monthly Income (Million VNDb) < 10 10 – 20 20 – 30 > 30 |
1309 1318 337 346 |
39.5 39.8 10.2 10.5 |
|
Sources of Information about COVID-19 Vaccine Radio/newspapers (yes) Television (yes) Internet/Social media (yes) Family/Friends/Colleague (yes) Healthcare professional/Hospital (yes) Public health/Government agencies (yes) Academic document (yes) |
244 1542 2881 1405 1634 1503 17 |
7.4 46.6 87.0 42.4 49.4 45.4 0.5 |
|
Chronic Diseases Cardiovascular (yes) Respiratory (yes) Endocrine (yes) Digestive (yes) Musculoskeletal (yes) Immune (yes) Others (yes) |
256 109 186 355 143 62 239 |
7.7 3.3 5.6 10.7 4.3 1.9 7.2 |
|
Number of Undergoing Diseases None 1-2 ≥ 3 |
2264 980 66 |
68.4 29.6 2.0 |
|
History of Taking other Vaccines No Yes |
600 2710 |
18.1 81.9 |
|
Perceived Health Status Good/Very good Fair/Poor/Very poor |
2076 1234 |
62.7 37.3 |
|
Existing of Infected Cases (250m radius) Currently Existing Ever Existed Not yet Existed |
1477 904 929 |
44.6 27.3 28.1 |
|
Regular COVID-19 Testing No Yes |
1295 2015 |
39.6 60.9 |
| Items | n (%) | Mean ± SDa |
|---|---|---|
| Knowledge (Correct Answer) | ||
| Current specific treatment for COVID-19 | 2368 (71.5) | - |
| The most effective method of preventing COVID-19 | 3152 (95.2) | - |
| COVID-19 can cause fatal if acquired | 3094 (93.5) | - |
| People without chronic diseases could get worsen or die with COVID-19 | 2947 (89.0) | - |
| People have more likely to get COVID-19 | 3274 (98.6) | - |
| Total score of knowledge | - | 4.48±0.73 |
| Sufficient knowledge (4-5 score) | 2984 (90.2) | - |
| Insufficient knowledge (0-3 score) | 326 (9.8) | - |
| Health Belief Model’s Components | ||
| Perceived Susceptibility | ||
| I have a high chance of getting COVID-19 | - | 3.77±0.97 |
| The COVID-19 pandemic has disturbed my life | - | 4.18±0.84 |
| I feel very worried about the current COVID-19 situation | - | 4.23±0.82 |
| I feel very worried if I get COVID-19 | - | 4.09±0.94 |
| Mean score of perceived susceptibility | - | 4.07±0.65 |
| Perceived Severity | ||
| The health condition or complication of being infected by the SARS-CoV-2 virus is very serious | - | 3.87±0.97 |
| I believe that I have good immunity against the SARS-CoV-2 virus | - | 3.26±0.98 |
| I believe that if I get COVID-19 this will be a serious health problem for me | - | 3.74±0.96 |
| Mean score of perceived severity | - | 3.62±0.70 |
| Perceived Benefits | ||
| Getting vaccinated is the right thing to do because it makes me less worried about getting COVID-19 | - | 4.27±0.87 |
| Getting vaccinated would help reduce my chances of getting COVID-19 or complications | - | 4.26±0.82 |
| Only people who are at high risk for COVID-19 need to be vaccinated against COVID-19 | - | 4.21±0.88 |
| Vaccination will help us quickly return to normal life | - | 4.08±0.92 |
| Mean score of perceived benefits | - | 4.21±0.63 |
| Perceived Barriers | ||
| I am afraid of needles | - | 2.06±1.01 |
| I am worried about possible serious side effects after getting COVID-19 vaccinated (vaccine safety) | - | 3.49±1.05 |
| I am worried that COVID-19 vaccine side effects may affect my daily activities | - | 3.21±1.08 |
| COVID-19 vaccine is too new for me to trust and decide to get vaccinated | - | 2.68±1.04 |
| I wonder about COVID-19 vaccine efficacy | - | 2.89±1.07 |
| Mean score of perceived barriers | - | 2.87±0.76 |
| Cues to Action | ||
| People having similar characteristics and around me have been vaccinated against COVID-19 | - | 3.62±0.81 |
| Everyone in the community is responsible for controlling the spread of the virus | - | 4.40±0.78 |
| I agree to get vaccinated when recommended by a healthcare professional | - | 4.24±0.75 |
| I agree to get vaccinated when recommended by the Government | - | 4.11±0.84 |
| I agree to get vaccinated once I fully understand about it | - | 4.34±0.68 |
| Mean score of cues to action | - | 4.14±0.56 |
| Characteristics | Acceptance | |||
|---|---|---|---|---|
| Acceptance | Not acceptance | χ2 or t value | p | |
|
Age (years) 18 – 39 40 – 59 ≥ 60 |
2190 (86.9) 642 (90.2) 74 (93.7) |
329 (13.1) 70 (9.8) 5 (6.3) |
8.010 | 0.018* |
|
Gender Male Female |
1016 (87.6) 1890 (87.9) |
144 (12.4) 260 (12.1) |
0.072 | 0.781 |
|
Education Level ≤ High school Vocational, school/college/University ≥ Post-graduate |
170 (85.4) 2004 (86.9) 732 (91.0) |
29 (14.6) 303 (13.1) 72 (9.0) |
10.823 | 0.004* |
|
Ethnicity Kinh Ethnic minorities |
2784 (87.7) 122 (91.0) |
392 (12.3) 12 (9.0) |
1.377 | 0.282 |
|
Religion/Religious Belief Buddhism Christian Others None |
486 (89.7) 324 (85.7) 33 (91.7) 2063 (87.6) |
56 (10.3) 54 (14.3) 3 (8.3) 291 (12.4) |
3.859 | 0.277 |
|
Marital Status Unmarried/widowed/divorced Married |
1258 (85.6) 1648 (89.6) |
212 (14.4) 192 (10.4) |
12.122 | 0.001* |
|
Geographic Zone Ho Chi Minh City Others |
2368 (87.8) 538 (87.6) |
328 (12.2) 76 (12.4) |
0.021 | 0.891 |
|
Region of Residence Urban Rural |
2596 (87.7) 310 (88.6) |
364 (12.3) 40 (11.4) |
0.220 | 0.730 |
|
Living Status Alone With clinically vulnerable people With others |
304 (86.1) 1544 (88.6) 1058 (87.1) |
49 (13.9) 199 (11.4) 156 (12.9) |
2.407 | 0.300 |
|
Occupation Student Healthcare-related worker Professional/Technician Public servant/ Self-employed/Others Housewife/Retiree |
333 (87.4) 1239 (91.4) 716 (84.8) 533 (84.5) 85 (85.9) |
48 (12.6) 116 (8.6) 128 (15.2) 98 (15.5) 14 (14.1) |
30.612 | <0.001* |
|
Employment Status Unchanged From employed to unemployed From unemployed to employed |
2361 (89.4) 532 (81.8) 13 (68.4) |
280 (10.6) 118 (18.2) 6 (31.6) |
34.454 | <0.001* |
|
Monthly Income (Million VND) < 10 10 – 20 20 – 30 > 30 |
1120 (85.6) 1178 (89.4) 298 (88.4) 310 (89.6) |
189 (14.4) 140 (10.6) 39 (11.6) 36 (10.4) |
10.348 | 0.016* |
|
Sources of Information about the COVID-19 Vaccine Radio/newspapers (yes) Television (yes) Internet/Social media (yes) Family/Friends/Colleague (yes) Healthcare professional/Hospital (yes) Public health/Government agencies (yes) Academic document (yes) |
222 (91.0) 1383 (89.7) 2513 (87.2) 1251 (89.0) 1503 (92.0) 1352 (90.0) 12 (70.6) |
22 (9.0) 159 (10.3) 368 (12.8) 154 (11.0) 131 (8.0) 151 (10.0) 5 (29.4) |
2.500 9.666 6.690 3.529 52.828 11.975 4.721 |
0.127 0.002* 0.009* 0.068 <0.001* 0.001* 0.047* |
|
Number of Sources of Information about COVID-19 Vaccine ≤ 2 3-4 ≥ 5 |
1287 (84.8) 1128 (89.5) 491 (92.1) |
230 (15.2) 132 (10.5) 42 (7.9) |
25.193 | <0.001* |
|
Number of Undergoing Diseases None 1-2 ≥ 3 |
2028 (89.6) 824 (84.1) 54 (81.8) |
236 (10.4) 156 (15.9) 12 (18.2) |
21.512 | <0.001* |
|
History of Taking other Vaccines No Yes |
517 (86.2) 2389 (88.2) |
83 (13.8) 321 (11.8) |
1.812 | 0.190 |
|
Perceived Health Status Good/Very good Fair/Poor/Very poor |
1589 (88.0) 1047 (84.8) |
217 (12.0) 187 (15.2) |
15.963 | <0.001* |
|
Existing of Infected Cases (250m radius) Currently existing Ever existed Not yet existed |
1285 (87.0) 787 (87.1) 834 (89.8) |
192 (13.0) 117 (12.9) 95 (10.2) |
4.724 | 0.094 |
|
Regular COVID-19 Testing No Yes |
1105 (85.3) 1801 (89.4) |
190 (14.7) 214 (10.6) |
12.076 | 0.001* |
|
Knowledge Sufficient (≥ 4 score) Insufficient (≤ 3 score) |
2637 (88.4) 269 (82.5) |
347 (11.6) 57 (17.5) |
9.405 | 0.003* |
| Perceived Susceptibility a | 4.09±0.61 | 3.89±0.83 | 49.958 | <0.001* |
| Perceived Severity a | 3.64±0.68 | 3.50±0.81 | 15.480 | 0.001 |
| Perceived Benefits a | 4.27±0.56 | 3.78±0.86 | 140.538 | <0.001* |
| Perceived barriers a | 2.81±0.74 | 3.26±0.79 | 5.469 | <0.001* |
| Cues to action a | 4.20±0.50 | 3.70±0.71 | 68.246 | <0.001* |
3.2. Health Belief Model’s Component Analysis
The results on knowledge and the HBM components for acceptance of the COVID-19 vaccine are described in Table 2. The mean total knowledge score of the respondents was 4.48±0.73 (0-5), with 90.2% of them showing a good level of knowledge (>= 4 points). Though a predominance answered correctly the question about the vulnerable groups for coronavirus, 28.5% wrongly responded about current COVID-19 treatment. High perceptions of susceptibility and severity caused by COVID-19 and benefits of COVID-19 vaccines were revealed by considerably high mean scores at 4.07±0.65, 3.62±0.70, and 4.21±0.63 respectively, whereas the average mean score of perceived barriers stood at a lower value (2.87±0.76). Of note, among statements about barriers that may hinder respondents’ decision to vaccinate against COVID-19, concerns about vaccine safety and post-vaccinated side effects were reported by the largest part of individuals, with the highest mean score in this section at 3.49 (SD=1.05). Finally, high levels of cues to action were also found with a mean of 20.70±2.79.
3.3. COVID-19 Vaccination Acceptance and its Predictive Factors
Overall, most participants were willing to get COVID-19 vaccination (87.8%) (definitely and probably agree), while only a low rate at 4.9% refused (disagree and definitely disagree) (Fig. 1). Only 104 showed their definite refusal (3.8%). In addition, when asked whether they recommended their loved ones (in the absence of contraindications) to receive the vaccine, 88.5% showed definite and probable willingness and only 4.7% answered ‘no’.
Table 3 illustrates the comparison of respondents' willingness to get vaccinated against COVID-19 among population characteristics. Among several sociodemographic and health-related variables, ten factors were found to significantly affect the raters' intention, including age, education level, marital status, occupation, employment status, monthly income, sources of information about COVID-19 vaccine, number of undergoing diseases, perceived health status and regular COVID-19 testing. The proportion of participants holding sufficient knowledge was also significantly different between the two groups. A cluster of channels where they get updated with COVID-19 vaccine information was also found as significant predictors, listed as television, social media on the internet, healthcare professionals or hospitals, public health or government agencies, and academic articles, with all p < 0.05. Furthermore, there were statistically significant differences in comparison mean scores of 5 elements of HBM between acceptance and not acceptance groups (pr0 < 0.05).
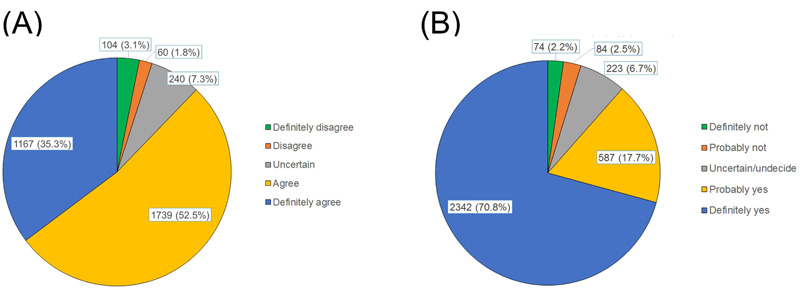
(A): Acceptance of COVID-19 vaccination
(B): Willingness to recommend ohters for COVID-19 vaccination.
The results of binary logistic regression analysis to define significant predictors of COVID-19 vaccination acceptance among demographic characteristics and the HBM components were presented in Table 4. The employment status changing from employed to unemployed, the number of chronic diseases, residing in areas with currently existing COVID-19 cases, concerns about health-related risks, doubtful safety, and inadequate information of this newly introduced vaccine were associated with increased refusal of COVID-19 vaccination, with all odds ratios lower than 1 and p < 0.05. In contrast, the number of platforms helping subjects stay updated with information about COVID-19 vaccine, holding positive perceptions on the benefits of COVID-19 vaccination, and having more cues to action was more likely to move towards acceptance of vaccination increased the acceptance rates (OR > 1, p < 0.05). On the other hand, this logistic regression analysis failed to find associations between the COVID-19 vaccine acceptance with the remaining demographic variables (p > 0.05).
| Characteristics | Acceptance | |
| ORa (95% CIb) | p | |
|
Age (years) 18 – 39 40 – 59 ≥ 60 |
0.41 (0.14–1.18) 0.54 (0.19–1.57) 1 |
0.098 0.258 |
|
Gender Male Female |
1 1.13 (0.88–1.45) |
0.354 |
|
Education Level ≤ High school Vocational, school/college/University ≥ Post-graduate |
1 0.83 (0.50–1.40) 0.86 (0.47–1.55) |
0.491 0.610 |
|
Ethnicity Kinh Ethnic minorities |
0.78 (0.40–1.52) 1 |
0.461 |
|
Religion/Religious Belief Buddhism Christian Others None |
1 0.72 (0.46–1.12) 1.79 (0.43–7.51) 0.78 (0.55–1.10) |
0.143 0.426 0.144 |
|
Marital Status Unmarried/widowed/divorced Married |
1 1.27 (0.96–1.68) |
0.089 |
|
Geographic Zone Ho Chi Minh City Others |
1.13 (0.80–1.62) 1 |
0.488 |
|
Region of Residence Urban Rural |
0.74 (0.47–1.16) 1 |
0.188 |
|
Living Status Alone With vulnerable people With others |
1 0.86 (0.57–1.29) 0.91 (0.61–1.35) |
0.469 0.624 |
|
Occupation Student Healthcare-related worker Professional/Technician Public servant/ Self-employed/Others Housewife/Retiree |
1 1.00 (0.62–1.61) 0.71 (0.45–1.12) 0.85 (0.53–1.38) 0.51 (0.23–1.16) |
0.999 0.141 0.518 0.107 |
|
Employment Status Unchanged From employed to unemployed From unemployed to employed |
1 0.70 (0.52–0.94) 0.33 (0.11–1.05) |
0.018* 0.060 |
|
Monthly Income (Million VND) < 10 10 – 20 20 – 30 > 30 |
1 1.21 (0.89–1.62) 0.95 (0.61–1.47) 1.11 (0.70–1.78) |
0.220 0.824 0.650 |
| Number of sources of information about COVID-19 vaccine | 1.10 (1.01–1.19) | 0.027* |
| Number of Undergoing Diseases | 0.76 (0.65–0.89) | 0.001* |
|
History of Taking other Vaccines No Yes |
1 0.89 (0.66–1.21) |
0.460 |
|
Perceived Health Status Good/Very good Fair/Poor/Very poor |
1.08 (0.84–1.40) 1 |
0.541 |
|
Existing of Infected Cases (250 m Radius) Currently existing Ever existed Not yet existed |
0.68 (0.50–0.93) 0.72 (0.51–1.01) 1 |
0.015* 0.057 |
|
Regular COVID-19 testing No Yes |
1 1.22 (0.95–1.58) |
0.118 |
|
Knowledge Sufficient (≥ 4 score) Insufficient (≤ 3 score) |
0.94 (0.65–1.36) 1 |
0.749 |
| Perceived Susceptibility | 1.01 (0.96–1.07) | 0.613 |
| Perceived severity | 1.04 (0.97–1.12) | 0.226 |
| Perceived benefits | 1.12 (1.07–1.18) | <0.001* |
| Perceived barriers | 0.88 (0.85–0.91) | <0.001* |
| Cues to action | 1.23 (1.18–1.29) | <0.001* |
Note: *p-value < 0.05
4. DISCUSSION
Up to the time of this study, Vietnam had been suffering the fourth hit of the COVID-19 pandemic and it had been the largest outbreak since the first proclamation of COVID-19 in January 2020. Also, the very first vaccines against COVID-19 began to be officially introduced to the Vietnamese at that time. Although mass vaccination for community immunity has proved its success in preventing the spread of transmissible diseases, refusal from getting vaccinated has posed a challenge to herd immunity, allowing preventable pathogens to persist in the population with inadequate vaccination rates. Being aware of this fact, in the face of the urgent situation of creating herd immunity to combat the pandemic, the Vietnam Government announced encouraging policies to promote residents’ vaccination acceptance. This study was conducted under such circumstances to investigate the public acceptance of COVID-19 vaccination.
The sample of this study has some features in accordance with the country’s demographics, in which the proportion of women was higher (65%) and the young age distribution (34.21±10.09) in this study was consistent with the data of Worldometer about Vietnam's population (50.1% and 32.5 years, respectively) [60].
Noticeably, since internet users were the target population, this study highlighted the widespread usage of social media on the internet as the most important channel for keeping updated with COVID-19 vaccine information, which was also noticed in other studies in Vietnam [46, 51] and Nigeria [36]. There was a significantly lower proportion of television utility to obtain news of the vaccines in this study (46.6%) compared to a previous study also in Vietnam (82.4%) [50]. It might be due to 76.1% of the current study sample aged 20-30. Staying informed by surfing the web has become a daily habit among the young population, which explains the internet as the most preferred information channel in this piece of work. Meanwhile, given the demographics as adults aged 52.9±15.6 years with undergoing chronic illness, it was not much surprising that the most preferred channel of information for Huynh et al.’s [50] subjects was traditional television, which understandably interpreted for this difference. Additionally, given that during the time of sampling, Ho Chi Minh City was the hardest hit place by the outbreak in Vietnam [61, 62], the considerable proportion of Ho Chi Minh citizens in this sample population was understandable. In addition, due to the nature of an online survey, urban citizens were likely to have a higher chance to access the questionnaire via the internet than rural people. Moreover, the majority of individuals residing in urban described in this study were also in agreement with that reported by Urrunaga Pastor et al. [63].
Of note, this study found a significantly higher percentage of acceptance of those accessing COVID-19 vaccine information through academic articles. Obviously, in the development process for any novel vaccine, certain phases need to be performed in an ordered and chronological pathway [64, 65]. Although certain stages might be simplified in the urgent need for a COVID-19 vaccine, results related to this process need to be reported through scientific articles, especially in major journals. In the context of the thirst for reliable information, thus, compared with traditionally given information, scientific results in prestigious journals have particularly high credibility, benefiting audiences in their decision-making to vaccinate. Therefore, this was reasonable that individuals tracking information through academic documents had a higher vaccination acceptance rate.
With 5 items measuring knowledge, most of the participants who submitted correct answers held sufficient knowledge related to the COVID-19 vaccine. The percentage in our study was significantly higher than previous studies with a wide range of individuals giving correct answers of 40.8% to 98.1% [51], 52.2 to 97.6% [46], and 40.0% to 93.2% [50]. These differences can be partially explained by looking at the characteristics of the subjects. While the participants in the reference studies were the elderly [50], with somewhat limited access to information, most of our subjects were young individuals and well-educated with at least a diploma degree, working as healthcare practitioners or in medical-related fields, professionals, or technicians, which all enabled them to have faster and more accurate approaches to information. Moreover, in contrast to the provincial-sited study of Nguyen et al. [51], most of the current participants resided in the most dynamic Ho Chi Minh City, which also partly reflected individuals' forceful access to the torrential flow of information about COVID-19 vaccination campaigns, affecting their level of knowledge. Furthermore, the results of any study are likely to depend on the context and time when the study is performed. Compared to previous studies, this work was conducted when educational information about COVID-19 vaccination was introduced to the community more abundantly and regularly than ever since Ho Chi Minh City had been the most seriously attacked by the 4th COVID-19 wave, compared to other neighboring provinces. This demonstrated the influence of long exposure and density of information on the community's knowledge.
Regarding domains of the HBM, the findings presented significantly higher mean scores of all domains than the other two studies conducted in Vietnam [50, 51]. Similar trends were observed in parts of cues to action and perceived benefits with higher mean scores in this study (4.14±0.56 and 4.21±0.63, respectively), compared to the referred studies (4.0±0.6 and 3.1±0.7 by Nguyen et al. [51] and 3.96±0.51 and 2.78±0.83 by Huynh et al. [50]). Up to the time of this study, the terrible severity in terms of the pandemic's spreading speed, fatality, and vulnerability was undoubtful. The community, therefore, witnessed the unprecedentedly serious susceptibility and severity caused by the pandemic. On the other hand, as indicated in Table 2, despite doubts about the vaccine's protective efficacy (2.89±1.07), respondents seemed to be more concerned about its safety or side effects (3.49±1.05). These results were in agreement with findings that concern for vaccine side effects was the most significant determinant of a higher likelihood of refusal [66], which suggested that besides educating about vaccine effectiveness against COVID-19, correct information about its side effects should be emphasized to promote the public’s acceptance. Moreover, while the higher the mean score implied the greater the level of hindrance, this study showed a significant perception of barriers (2.87±0.76) than the previous one (2.4±0.5) [50].
It is understandable that at the time of Nguyen et al.'s study [51], the first batch of the COVID-19 vaccine in Vietnam was just assigned to very few prior frontline personnel engaged in the COVID-19 battle but not widely offered for the community [67, 68]. This means that unexpected information about the vaccine and its post-injection effects was not too common in Vietnam, partly illuminating for the negligible level of community concerns then.
In contrast, when the current study survey was disseminated to the target population, the vaccination campaign had already occurred over a certain period. The entire public’s interest seemed to focus on the safety of vaccine first doses in humans and the worrying reported numbers of deaths or serious complications after their emergent use, not only in the world but also in Vietnam [69-71]. Therefore, instead of properly understanding the prevalence of these side effect events, which represented a very small and unsubstantial percentage relative to the vaccinated population, the community had become obsessed with concerns about these misinterpreted figures. In addition to the lack of properly explanatory information for reference provided by healthcare professionals or trustworthy channels, this phenomenon was also influenced by the complexity of the medical specialty, which might require a certain level of knowledge of the audiences. Moreover, seeing reports of adverse reactions or deaths caused by anaphylaxis following COVID-19 vaccination led the community witnesses, mostly without health science knowledge, to worry about its safety, resulting in a higher anxiety score as well.
Regarding the acceptance of the citizens to take the COVID-19 vaccine, this study showed a much higher acceptance rate (87.8%) than other studies conducted in Vietnam or other regions, which reported vaccination intention rates ranging from 27.7% - 83.8% [16, 20, 21, 24, 26, 27, 29, 31, 38, 39, 42, 44, 45, 51, 72]. The cited works and the current ones were similar in the justification for the differences in the HBM domains scores. However, while the vaccine was not introduced to recipients but only through social media or clinical trial results at the time of the previous studies, the participants in our work had real experiences with the COVID-19 vaccine, in which people around them were vaccinated in turn. This could be the most plausible explanation for the aforementioned difference.
Furthermore, the onslaught of the fourth COVID-19 wave at the time of this study partly convinced the participants to choose in favor of vaccination when they weighed between subjective concerns and rare consequences and the unambiguously devastating impact of the pandemic. Additionally, this acceptance rate was lower than a study conducted in March 2020 in the Chinese community, with 91.3% [37]. Wang et al. introduced the survey when China was in an unprecedented state of turmoil due to the COVID-19 pandemic, with the first-ranked number of cases and deaths worldwide [72, 73]. These life-threatening events possibly influenced these people's choice of life pursuits, which was also observed in the present study. Considerably, at that point of the survey, Vietnam only approved the emergency use of 3 vaccines provided by the world's leading vaccine and pharmaceutical manufacturers, Oxford/AstraZeneca COVID-19 vaccine, Pfizer-BioNTech COVID -19 Vaccine, and Moderna COVID-19 vaccine [74]. The beliefs in the safety and effectiveness of these vaccines, combined with the urgent need for community immunization also explained the high vaccination acceptance rate of the participants in this study.
When looking at the willingness to encourage others to vaccinate, a similarly high proportion (88.5%) of acceptance was observed. Interestingly, despite only 35.5% being definitely willing to get vaccinated for themselves, the number answering “definitely yes” to recommend their family, friends, or others to take COVID-19 vaccination climbed up to 70.8%. Viewing from the personalized aspects, human nature was understandable to hesitate and take a more cautious attitude to decide when facing a dilemma between vaccine efficacy and safety. They preferred to wait for others’ vaccination experience as a prior reference [66]. Therefore, it was possible to partly clarify their stronger preferences for the vaccination of their friends or others.
The present study revealed some significantly relative determinants that describe respondents as “vaccination advocators”. Similar to previous studies [16, 20, 25, 46, 47, 51, 53, 75], we also found positive associations of vaccination probability with perceived benefits and cues to action and a negative one with perceived barriers. These correlations fitted and followed the HBM [54, 55] cited in previous studies [37, 46, 50, 51]. A person would be likely to commence a suggested preventive health action when they were aware that their health was being threatened or progressively cued to action, or the perception of benefits they got was heavier than the barriers [76].
Another positive correlation between the number of sources of information and intention to receive vaccination was also observed. Unsurprisingly, by early accessing more information sources, especially accurate and updated news broadcasted by official providers, audiences' knowledge and positive perception of COVID-19 vaccines were further improved the most effectively, subsequently navigating them to the more intelligent choices of vaccination. This encourages the active running of providing authoritative information, which would take advantage of diverse communitive platforms to keep the community informed and make rational decisions towards their vaccination.
However, there were unpredictable results of negative correlations of vaccine willingness with the employment status change from employed to unemployed, current circulation of COVID-19 in participants’ residents, and the number of chronic illnesses. It was logically anticipated that unemployed people tended to accept vaccination so that they could return to normal life soon. Nonetheless, people experiencing unemployment due to COVID-19, especially in the situation of the city curfew and lockdown policies, were mostly grouped as unprofessional with lower literacy levels, such as public servants or general workers. As a result, the knowledge and perception convincing them to get vaccinated were prone to be less sufficient than those with essential professional or higher education.
Similarly, people with more chronic diseases are often elderly with less accurate access to information and in a more passive way. Furthermore, given some worrying news about the side effects of the vaccines, these people, by their nature of poor health and belonging to the vulnerable population, seemed to face higher hesitancy, which explained why the higher number of chronic diseases they got, the lower possibility of vaccination acceptance. This was also consistent with the result that more consideration of vaccine side effects and health risks made people more hesitant to vaccinate [66]. On the other hand, living in a “red zone” might make people afraid to step out of their houses, which they consider a safer environment to protect them from virus exposure. Thus, excessive fear could also be another reason for their going-out hesitation, including refusing to undergo grouped rapid testing or vaccination. In addition to insufficient awareness of the vaccine benefits, this could mislead them to believe that it would be better to stay at home without contacting anyone than to go out for vaccination and then get the risk of virus exposure and vaccine side effects. This might explain why people in “red zones” delayed their vaccination willingness.
4.1. Strengths
The large size of this study sample could be considered the first strength. Random sampling without geographical restrictions and disseminating the survey via online platforms yielded a broad coverage of participants from regions strongly affected by COVID-19 with various socio-economic characteristics. Additionally, the research was carried out in a context where vaccine development was no longer confined to the laboratory but at the beginning of actual vaccination campaigns. Therefore, the responses based on the real-time experiences of this study’s participants provided more accurate and applicable reference information.
4.2. Limitations
Besides the strengths of an online tool able to reach the unlimited target population, information bias was somewhat unavoidable as a result of the self-reported nature, despite thorough instructions included at the beginning of the questionnaire. In addition, due to the limitation of closed contact during social distancing, face-to-face access for data collection was unfeasible. Therefore, it is undeniable that the study missed some social classes of the public who were unfamiliar with social networks or smart devices to access the survey link, such as those in low socioeconomic short.
Besides restricted direct contact, online disseminating the survey widely to the population was also difficult because, at this point, the information crisis related to COVID-19 was at its peak, making people confused, overloaded, and saturated with too many streams of information. Therefore, snowball sampling, which was also applied in other works [20, 25, 36, 39, 53], was considered the most appropriate approach despite some disadvantages. This method is non-probability, leading to uncalculated sampling error and highly possible bias. Specifically, this study started the participant recruitment from the researchers' networks, mostly healthcare-related workers. As a result, the sample skewness to groups with better education and working in healthcare-related fields lead to the limited representativeness of this study. These inevitable biases in which some respondents were over-represented in the sample were also observed and acknowledged in some studies that applied the same sampling technique [20, 25, 36, 39, 53].
Despite these mentioned weaknesses, to some extent, this study was valuable for the initial assessment of a specific part of the Vietnamese population regarding COVID-19 vaccination acceptance. Somehow, healthcare workers and those who are knowledgeable about healthcare are an important influence on public perception of the COVID-19 vaccine. Initially, evaluating and finding ways to strengthen their right attitudes about vaccination would be helpful in spreading the right knowledge to the community.
CONCLUSION
Vaccine undoubtedly receives a high agreement about its crucial role in controlling and eradicating a series of transmissible diseases. The vaccine uptake acceptance rate and its predictors in the present study reflected a general picture of the community’s awareness and action orientation on COVID-19 immunization. The level of participants’ acceptance of COVID-19 vaccination in this study was impressively high, reflecting the efforts of health authorities and the government. The contribution of influential healthcare professionals or authoritative information to vaccination probability implied that in order to achieve significant and rapid results, educational information about COVID-19 vaccines should be widely broadcasted in prominent communication channels such as social media platforms and television by a combination of government and influenceable healthcare providers from medical institutions. It also highlighted the role of citing reliable scientific articles while informing the public to build their confidence in vaccine safety. Moreover, through the study results, during the design of these immunization campaigns, governments and health care managers should pay more attention to people with low acceptance levels, such as chronically ill adults, and rectify confusing information to correct the public’s awareness about immunization and herd immunity benefits. Moreover, the design of educational campaigns for herd immunity against COVID-19 should focus more on offering accurate information about the side effects and safety.
LIST OF ABBREVIATIONS
| aSD | = Standard Deviation |
| bVND | = Vietnam dong |
| aOR, odds ratio; 95% bCI | = 95% Confidence Interval |
ETHICS APPROVAL AND CONSENT TO PARTICIPATE
Before its data collection stage proceeded, this study was ethically approved by the Medical Ethics Committee. It had ethically approved this study of University Medical Center Ho Chi Minh City, Vietnam, before its data collection stage proceeded (Approval No.77/GCN-HĐĐĐ-UMC, 26/7/2021).
HUMAN AND ANIMAL RIGHTS
No animals were used in this research. All human research procedures followed were in accordance with the ethical standards of the committee responsible for human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2013.
CONSENT FOR PUBLICATION
The respondents were first required to show their consent by answering a required question in the introductory part of the survey if they were willing to go through the survey as a participant in the study.
STANDARDS OF REPORTING
STROBE guideline has been followed.
AVAILABILITY OF DATA AND MATERIALS
The supportive data of the results of this study are available within the paper.
FUNDING
None Declared.
CONFLICT OF INTEREST
The authors declare no conflict of interest, financial or otherwise.
ACKNOWLEDGEMENTS
The authors sincerely thank all participants for their assistance completing this study and disseminating it to other potential participants.


